Your doctor tells you that you need a statin to lower your cholesterol and reduce your heart attack risk. You don’t like taking medicine and your friend tells you that he had achy muscles after he started a statin. You wonder if you should listen to your doctor or go without the medicine. An article just published in Mayo Clinic Proceedings by Dr. Carl E Orringer of the University of Miami Miller School of Medicine and Dr. Kevin C Maki of Indiana University’s School of Public Health may help your doctor to make the right decision.
The American Heart Association, American College of Cardiology and 10 other medical organizations published a Guideline in late 2018 to help doctors determine which patients are most likely to benefit from cholesterol-lowering drug treatment. Statins, the most widely prescribed cholesterol-lowering medicines, have well-established benefits for lowering heart attack and stroke risk.
For those who don’t have a previous history of cardiovascular disease or other high-risk conditions, the Guideline recommends that doctors use a risk calculator to help to decide which patients have high enough cardiovascular risk to benefit from a statin. A statin is recommended for those at high risk, and not recommended for those at low risk. However, most have risk somewhere in between, where the decision about the need for statin treatment is uncertain.
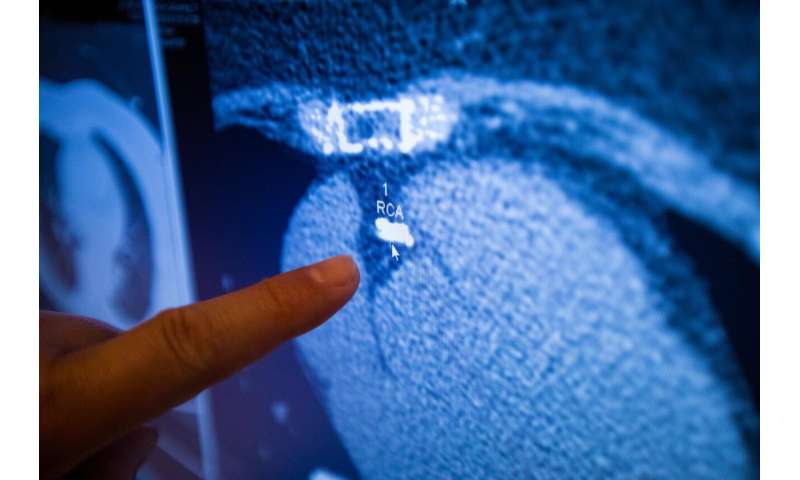
An imaging test called coronary calcium scoring can help doctors to make the right recommendation about the use of statin therapy. The test is a 10-minute CT (computed tomography) scan looking for calcium deposits in the arteries supplying blood to the heart. Calcium deposits indicate the presence of coronary plaque, also known as atherosclerosis.
The test requires no injections, produces less radiation exposure than a routine mammogram, and is widely available, usually costing $99 or less. This test has been available for about 20 years, but its use to guide treatment decisions for heart attack and stroke prevention has only recently been supported by enough evidence to recommend widespread use.
Up to half (generally 40-50%) of people with a calculated heart attack and stroke risk in the middle group between the low and high categories have a calcium score of zero. These people have such low heart attack and stroke risk over the next 10 years that taking a statin provides, at most, minimal protection. On the other hand, those with evidence of significant calcium build-up are very likely to benefit from taking a statin.
Taking a statin is not a small decision, since doing so means that buying the medicine, taking it daily, and undergoing follow-up blood tests and medical appointments to be sure that the treatment is working. In addition, a small percentage of patients have side effects that may require additional testing and medical appointments. That is why Drs. Orringer and Maki make the point in this article that coronary calcium scoring in this “middle risk” group is so important. They recommend that patients in this group get the test, whenever possible, so that therapy can be more effectively targeted to those most likely to benefit. KCM: The preceeding paragraph could be omitted if we want to keep to one page.
Cardiovascular diseases such as heart attack and stroke are the leading causes of death for both men and women in the United States. An important point made in the article is that coronary calcium scoring may be particularly useful in women 50 years of age and older. There is more than a 50% chance that a woman in her 50s will eventually develop cardiovascular disease. The risk of developing breast cancer over a lifetime (about 12-13%) is much lower than for cardiovascular disease. Women who are 55 years of age or older and at average breast cancer risk are advised to have a screening mammogram annually, or every other year.
Source: Read Full Article