In July, New York State health officials notified the Centers for Disease Control and Prevention (CDC) of a case of paralytic polio in an unvaccinated adult in Rockland County, N.Y. Wastewater samples from communities near the patient’s home confirmed that poliovirus was present in those areas. The virus has been found in wastewater samples in New York City, as well.
Polio was once one of the most feared diseases in the United States, according to the CDC. The polio vaccine used in the United States protects against severe disease in nearly everyone—99 out of 100 people—who has received all four recommended doses. Among U.S. kindergarten students, the CDC reports that 93% had received all four doses by the 2020-21 school year. But the statewide polio vaccination rate in New York state was under 79%.
Despite the renewed threat, the latest Annenberg Science Knowledge (ASK) national panel survey by the Annenberg Public Policy Center finds that a sizable portion of the U.S. public is unfamiliar with the risks of polio.
The latest survey, conducted in October, examines public knowledge and beliefs about the poliovirus, the bivalent COVID-19 vaccine booster, monkeypox, and other matters of public health.
Among the findings:
- Only a third of U.S. adults (33%) know there is no cure for polio—and over 1 in 5 U.S. adults (22%) do not know whether they’ve been vaccinated against polio.
- Far more people report support for taking the vaccines against polio or monkeypox than the updated COVID bivalent booster (see question wording below).
- Few people regard the updated vaccine as less safe or efficacious than the original COVID vaccine—just 7% think it is less safe than the original while 8% consider it is less effective than the original.
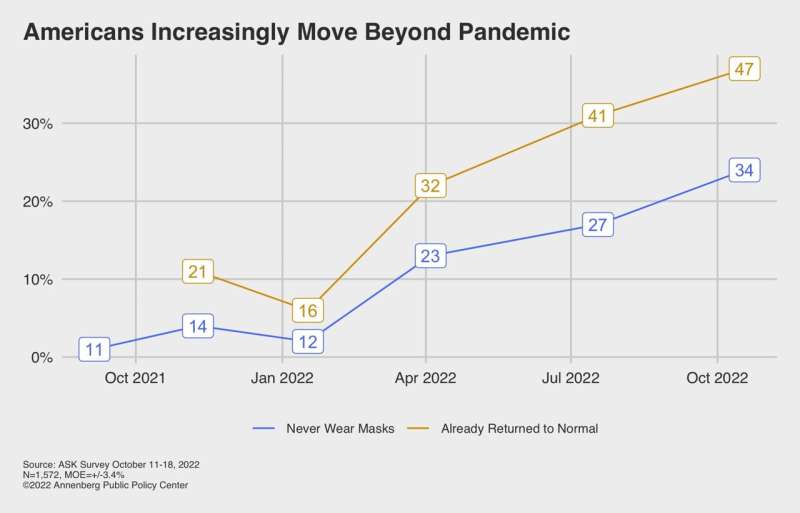
- Almost half of American adults (47%) say they have returned to living their normal, pre-COVID lives, up from 41% in July.
“The victory over polio is one of the great medical achievements of the 20th century,” said Kathleen Hall Jamieson, director of the Annenberg Public Policy Center. “It would be tragic if under-vaccination were to jeopardize that accomplishment.”
The nationally representative panel of 1,572 U.S. adults surveyed by SSRS for the Annenberg Public Policy Center of the University (APPC) of Pennsylvania from October 11-18, 2022, was the ninth wave of an Annenberg Science Knowledge survey whose respondents were first empaneled in April 2021.
What the public knows about polio
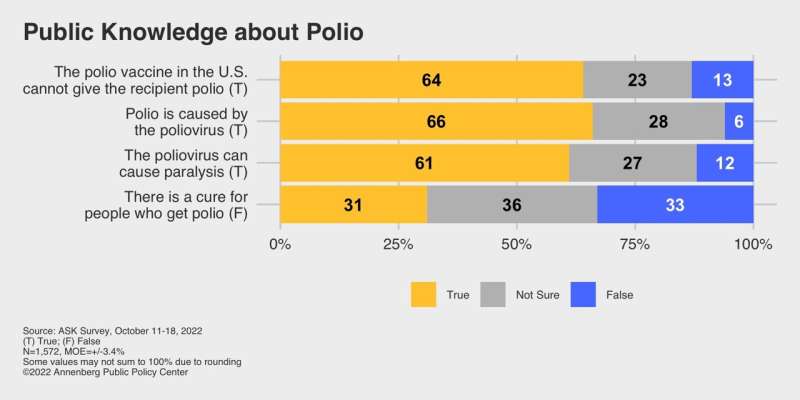
The latest wave of the ASK survey finds that much of the public is knowledgeable about certain aspects of polio but there are substantial levels of uncertainty:
- Two-thirds of those surveyed (66%) know it is true that polio is caused by the poliovirus, though 28% are not sure if this is true.
- 64% know it is true that the polio vaccine administered in the United States cannot give a recipient polio (since 2000, only an inactivated polio vaccine has been used in the United States), though 23% are not sure.
- 61% know the poliovirus can cause paralysis, though 27% are not sure.
- But only a third of those surveyed (33%) know there is no cure for polio; 31% incorrectly think there is a cure and 36% are not sure.
Higher risk for polio: Most of the survey respondents are unsure about practices that would put a person at higher risk for contracting polio:
- Less than a third (31%) know that people are at higher risk of infection with poliovirus if they are in contact with droplets or sneezes from an infected person. But over half (58%) are not sure.
- Just a quarter (25%) know that people are at higher risk of infection with poliovirus if they consume contaminated food or water, while over half (58%) are not sure.
- Just a quarter (25%) know a person is at higher risk of infection with poliovirus if they are in contact with the stool of an infected person, while two-thirds (65%) are not sure.
Vaccination for different diseases
This fall, the CDC recommended a bivalent mRNA COVID-19 vaccine booster dose for people ages five and older, to be given at least two months after the primary vaccine series or another booster (the CDC also says “you may consider delaying” a vaccine primary dose or booster three months after symptomatic COVID or a positive COVID test).
The bivalent booster is designed to target the original version of the coronavirus that causes COVID-19 as well as two omicron subvariants. The two subvariants accounted for most cases in the United States as of late August.
Although survey respondents overwhelmingly say they do not have concerns about the safety or effectiveness of the new booster, they show much less acceptance of it than the vaccines against polio or monkeypox:
- 85% say they are likely to recommend that an eligible person in their household get vaccinated with the polio vaccine.
- 76% say that if exposed to monkeypox they would be likely to take the monkeypox vaccine, which can be given after exposure (ideally, within four days).
- But less than half (45%) say they are likely to get the updated mRNA COVID booster if eligible to get it, about even with the 42% who say they are unlikely to get it.
While interest in getting the COVID booster is weaker than for some other vaccines, the survey respondents think that younger and older people would benefit from getting it.
The survey finds that 60% of the public says that if someone in their household was 5 to 18 years old, they’d be likely to recommend that that person get the updated COVID-19 booster (asked of a subsample). More (69%) say it’s likely that a healthy young person would benefit from getting the new booster, which targets both the original coronavirus and the BA.4 and BA.5 variants. Nearly 4 out of 5 people (79%) say it’s likely that a person over 65 years old would benefit from taking the booster.
Despite the lower level of support for the COVID booster, the public has few safety or efficacy concerns about it. Only 7% think it is less safe than the original COVID vaccine, while 60% in total think it is either as safe (48%) or more safe (12%) than the original. Only 8% think the new booster is less effective than the original, while 58% in total think it is either as effective (37%) or more effective (21%) than the original. In both questions, about a third of respondents are not sure.
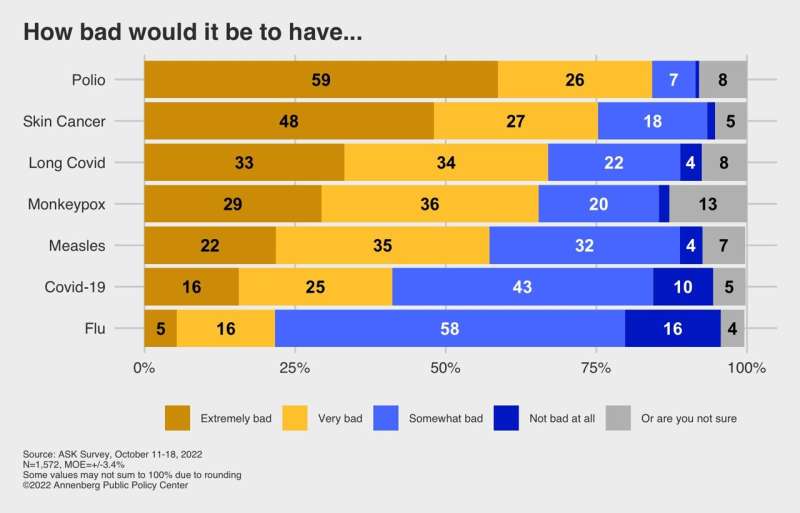
How bad would it be to get … polio? Monkeypox? Long COVID?
There is greater concern about getting “long COVID,” the series of lingering harmful effects such as fatigue and neurological problems that may follow infection with COVID-19, than with getting COVID-19 itself. Asked how bad it would be to have different diseases and illnesses, the public sees long COVID as not as bad as skin cancer but as bad as monkeypox and worse than measles:
- 84% think it would be extremely or very bad to have polio
- 75% think it would be extremely/very bad to have skin cancer
- 67% think it would be extremely/very bad to have long COVID
- 65% think it would be extremely/very bad to have monkeypox
- 57% think it would be extremely/very bad to have measles
- 41% think it would be extremely/very bad to have COVID-19
- And 22% think it would be extremely/very bad to have seasonal flu.
“With uptake of the bivalent vaccine worrisomely low,” Jamieson noted, “it is important that the public know that some studies have found the risk of long COVID is lower after vaccination.” Under 12% of the U.S. adult population has had the updated bivalent booster, the CDC says.
The relatively lower level of concern with getting COVID may reflect our survey respondents’ real-world experience: 47% of our survey panel say they have tested positive for COVID-19 and 23% of this COVID-positive group has had it more than once (which is equivalent to 11% of the overall U.S. population). Far fewer people (6%) say they have or have had long COVID (11% are not sure). A larger group of respondents (29%) know someone who has experienced long COVID.
The CDC said estimates of how many people develop long COVID symptoms vary widely depending on how a study was conducted: 13.3% had long COVID symptoms at one month or longer after infection; 2.3% reported symptoms at three months or longer; and over 30% at six months among patients who were hospitalized.
A continuing return to normal
When asked when they expect to be able to return to their normal, pre-COVID-19 lives, nearly half of those surveyed in October (47%) say they already have, up from 41% in July, 32% in April, and 16% in January. Those who feel the return to normal is still more than a year away is down to 13%, from 19% in July.
Source: Read Full Article