Benign breast diseases (BBD), which are non-cancerous disorders of the breast, such as lumps, are known to increase the chances of subsequent breast cancer. Now a team of Spanish researchers have found that the way BBD is detected as part of a national screening programme is an indication of which are more likely to become cancerous.
The findings from a team led by Professor Xavier Castells, head of the epidemiology department at the Hospital del Mar Medical Research Institute, Barcelona, Spain, will be presented at the 12th European Breast Cancer Conference on Saturday.
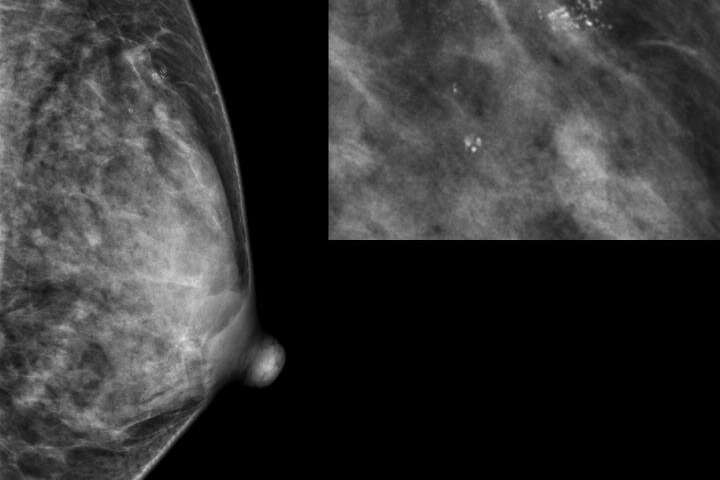
BBD detected on the first occasion a woman attends for breast screening (usually at the age of 50 in Spain and many other European countries with national screening programmes) is classified as “prevalent” BBD, whereas those detected on subsequent visits, which occur every two years in Spain, are classified as “incident” BBD.
Dr. Marta Román, a senior researcher in the epidemiology department at the Hospital del Mar Medical Research Institute, told the conference: “Our results show that women with a benign breast disease diagnosed from the second screening onwards have a significantly higher subsequent risk of breast cancer than those with a BBD diagnosed on their first mammographic screening.”
The researchers analysed data from 629,087 women who underwent 2,327,384 screening mammograms between 1995 and 2015, and they followed them until 2017. They found that women diagnosed with incident BBD had a 2.67-fold increased chance of developing breast cancer than women with no BBD, while women with prevalent BBD had a 1.87-fold increased risk.
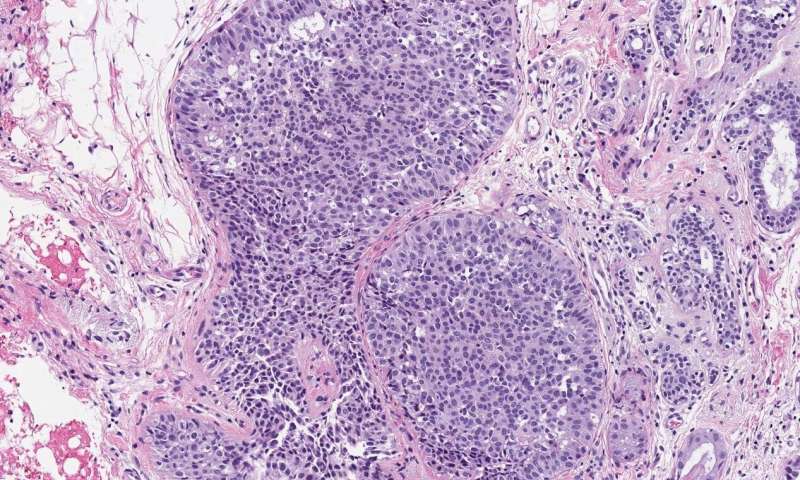
They also classified the BBDs as non-proliferative or proliferative, depending on whether or not the breast tissue showed an increase in the growth of certain cells, such as the ductal cells found in ductal hyperplasia in which there is an overgrowth of cells lining the ducts inside the breast.
They found that women with proliferative BBD had a 3.28-fold increased chance of breast cancer compared to women with no breast disease, while women with non-proliferative BBD had a 1.96-fold increased risk.
Dr. Román said: “We found the highest risk of breast cancer in women with incident, proliferative BBD. They had a nearly four-fold increased risk of breast cancer compared to women with no BBD.”
Women with an incident, non-proliferative BBD had a 2.39-fold increased chance of subsequently developing breast cancer compared to women with no BBD; women with prevalent, proliferative BBD had a 2.85-fold increased risk; and women with prevalent, non-proliferative BBD had a 1.63-fold increased risk.
The researchers hope that their findings will be useful in designing personalised breast cancer screening strategies in order to improve the effectiveness of breast cancer screening.
“The likelihood that a woman will benefit from screening mammography depends on her risk for developing clinically significant breast cancer in her lifetime,” said Dr. Román. “Taking individual risk factors beyond age into account should enable the classification of women into groups at varying risk of breast cancer. Personalised risk-based screening going beyond the current ‘one-size fits all’ recommendation may increase the effectiveness of breast cancer screening. Including information from BBD, in addition to other factors, to develop risk-based screening approaches can help with the prediction of whether a woman would develop breast cancer in a defined period.
“Different screening strategies can be considered for each woman based on her personal risk of breast cancer: by modifying the screening interval, which could be annual, or every two or three years, the method of screening, for instance, mammogram, ultrasound or magnetic resonance imaging, or the age range in which the woman is invited for screening participation.”
Dr. Román and her colleagues believe these findings will help clinicians to understand the different risks associated with BBD and to improve the accuracy of breast cancer risk predictions.
In a statement before the conference, Professor Xavier Castells said: “Clinicians involved in the management of women with BBDs could offer targeted surveillance strategies considering, in addition to other factors, if the BBD was found at first or in subsequent screening examinations. Also, this information will be included in an individualised model that can be used to predict an individual woman’s risk of developing breast cancer in five or ten years’ time. We have tested this in the context of a screening programme, which also includes information on breast density, age, family history of breast cancer and mammographic features.”
The team is part of MyPebs: an international randomised controlled trial, funded by the European Union that investigates whether a risk-based breast cancer screening strategy, based on a clinical risk score, is more effective than standard screening. This international project, which started in July 2019, will recruit 90,000 participants from six countries and follow them for four years.
Co-chair of EBCC12, Professor Javier Cortes, is clinical investigator of the breast cancer research programme at Vall d’Hebron Institute of Oncology, Barcelona, and head of the breast cancer programme at the IOB Institute of Oncology, Madrid and Barcelona, and was not involved with this research. He commented: “We know that population-based breast cancer screening programmes save lives by detecting cancer at an early stage. However, it can raise questions about not only the best way of treating women with cancer that may never become a problem in their lifetimes, but also what to do about women with benign breast disease.
Source: Read Full Article