In the next 20 years, there will be a substantial global rise in multimorbidities, with consequences for patients, caregivers, health care systems and society. Addressing this challenge requires a shift in the prevailing clinical, educational, and scientific thinking and organization.
In a review published July 18 in Nature Medicine, Professor Claudia Langenberg, Director of the Precision Healthcare University Research Institute (PHURI) at Queen Mary University of London; Professor Sir Chris Whitty, Chief Medical Officer for England; and Professor Aroon Hingorani, University College London suggest that a change to a data-driven approach is crucial to meet the challenge of multimorbidity.
Our current approaches to understanding and treating multimorbidity do not account for the ethnic and pathological diversity of multimorbidity that is present nationally or globally and the profound inequalities that exist within and between economies.
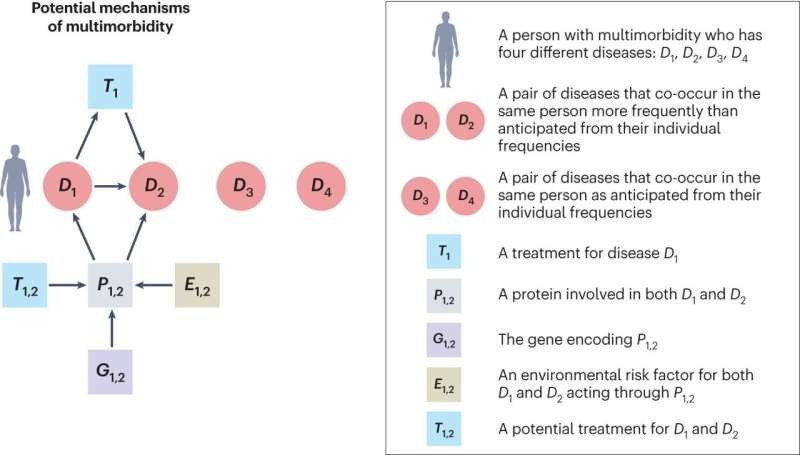
Multimorbidity is defined as “the simultaneous occurrence of two or more chronic conditions in the same individual, regardless of cause.” The authors argue that this definition should be changed to consider the occurrence of two or more conditions in the same individual, regardless of chronicity, over the person’s entire life.
“The current definition omits the fact that chains of causation may be separated in time, with acute, treatable, or self-limited conditions having consequences later in life,” says Professor Langenberg. “For example, survivors of Hodgkin’s lymphoma in childhood have a higher risk of cardiovascular disease and a second cancer in in the breast, lung, or thyroid in later life.”
We must shift our clinical, educational, and scientific approaches to meet the challenge of multimorbidity. Most of the existing research on multimorbidity focuses on a very small group of long-term conditions where age is the main driver of multimorbidity, neglecting thousands of conditions in the U.K. We must capitalize on advances in genomics and computing to gather information about how diseases interact. Data-driven scientific approaches could help to identify patterns, clusters and trajectories in multimorbidity, while considering data on life stages, ethnicities, sexes, socioeconomic groups and locations. This will be a key focus of Queen Marys Precision Healthcare University Research Institute.
Modern medicine is built around a single disease approach—how we train health care professionals, organize medical disciplines and write clinical guidelines are optimized for a single disease. Its a similar picture in scientific research, with academia, funding and study design usually organized around a single disease or organ. Multimorbidity is not a single entity but differs quantitively and qualitatively across life stages, ethnicities, sexes, socioeconomic groups, and geographies, and in order to better understand and treat multiple conditions, these must be considered. There is an urgent need for more systematic recognition of the interaction between diseases in research and their importance in clinical practice.
More information:
Claudia Langenberg et al, Biological and functional multimorbidity—from mechanisms to management, Nature Medicine (2023). DOI: 10.1038/s41591-023-02420-6
Journal information:
Nature Medicine
Source: Read Full Article