A recent review by a team of world leaders in Polycystic Ovary Syndrome (PCOS) research and care, led by Monash University, provides a summary of best practice evidence and advocates for greater funded research to address remaining gaps in knowledge in this often neglected condition.
The comprehensive review, now published in The Lancet Diabetes & Endocrinology, highlights the need for dedicated services and enhanced uptake of evidence-based resources to optimize best practice diagnosis, care and health outcomes in partnership with women. It also provides an up-to-date reference point for clinicians and other health professionals who provide healthcare to women with PCOS.
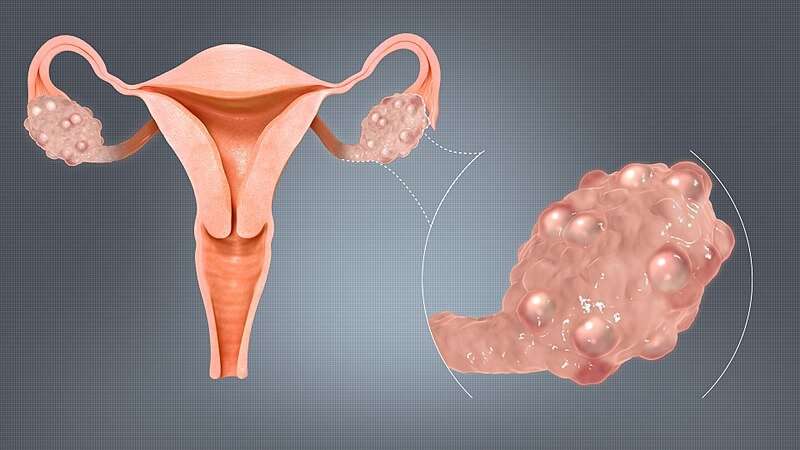
PCOS is a common condition that affects 8–13% of women. Diagnosis is often delayed, requires multiple consultations and is based on irregular periods, higher levels or signs of excess male type hormones, including excessive hair growth or severe acne, and ultrasound changes on the ovaries. The condition has metabolic, psychological and reproductive features and is one of the main causes of infertility in women.
Professor Helena Teede, from the Monash Center for Health Research and Implementation (MCHRI) says the review paves the way for the 2023 release of the International PCOS Guidelines, generously funded by the National Health and Medical Research Council (NHMRC) Center for Research Excellence in Women’s Health in Reproductive Life.
“There are key knowledge gaps that clinicians have when diagnosing and treating PCOS. The review seeks to improve accurate diagnosis, limit treatment inconsistencies and address barriers to providing patient centered care. It also highlights the need for holistic models of care to support women and for greater investment in research in this common, yet complex condition,” said Professor Teede.
Lorna Berry, 52, has PCOS and is a consumer lead on the International PCOS Guidelines.
Throughout her 20s and early 30s, Lorna went from doctor to doctor searching for answers and a diagnosis for her symptoms. By 32, feeling disappointed and unsupported, she self-diagnosed herself with PCOS.
“The voices of women with PCOS are so important, and it’s time we work with doctors to get the diagnosis and care right,” Lorna said. “PCOS isn’t just a condition that affects women during childbearing years but affects women their whole lives. We can’t let another generation of women go undiagnosed.”
Senior author and lead in the only dedicated holistic PCOS service in Australia, Dr. Anju Joham, based at Monash Health says: “Women want an accurate and more prompt diagnosis, so they can get on with adapting lifestyle factors and finding an effective, individual management plan. This requires effective translation tools and resources to educate the community, women and health professionals.”
In 2020, MCHRI researchers released the free, evidence-based AskPCOS App which has been co-developed with women and health professionals. It has 21,000 users across 178 countries and has significant information, a moderated discussion forum, symptom tracker, user-friendly infographics and tools to assist shared decision-making with healthcare providers. It was developed purely to inform women like Lorna and their healthcare providers, and to improve health outcomes.
Source: Read Full Article