In a recent study published in Nature Medicine, a team of researchers from different countries performed a meta-analysis of real-world cross-cohorts and provided an association of the gut microbiome with immune checkpoint inhibitors (ICIs) response in patients with advanced melanomas.
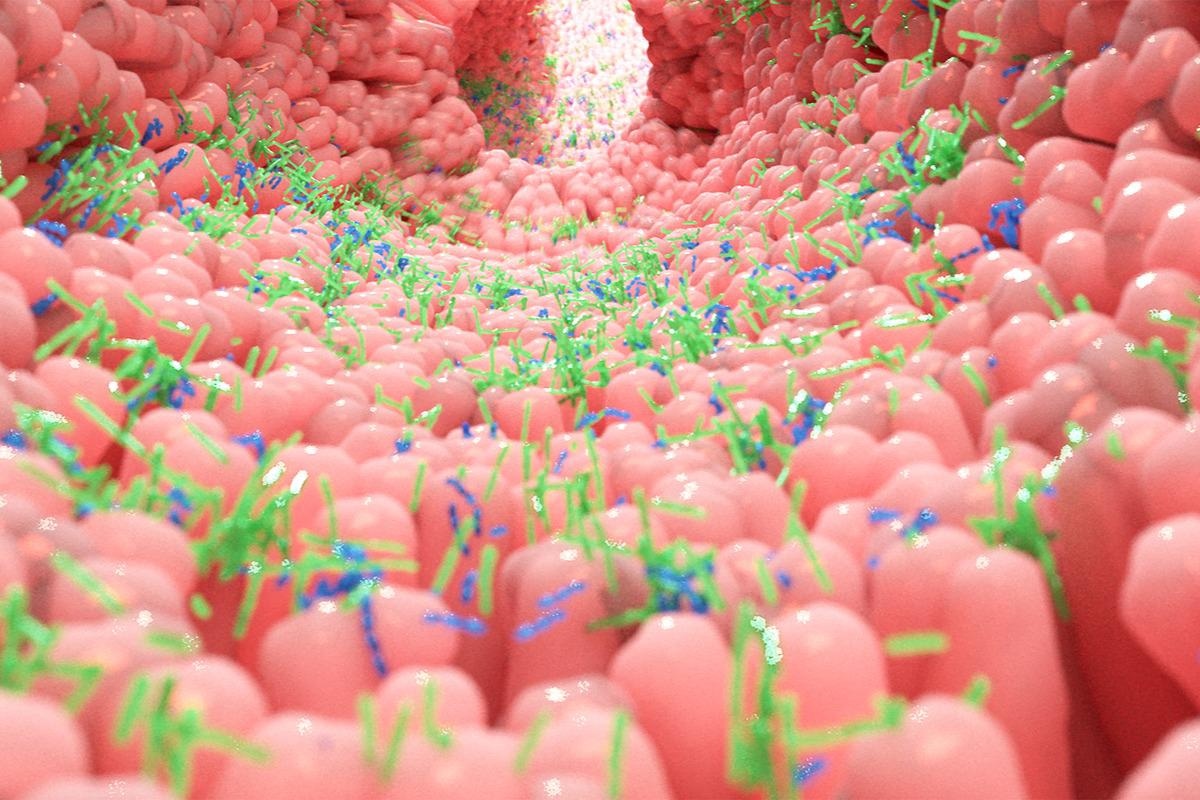
The treatment of advanced melanomas has revolutionized with the advent of ICIs that target immune checkpoints such as programmed cell death protein 1 (PD-1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). In patients treated with ICIs, gut microbiome composition has been associated with their clinical responses. However, limited data is available about the characteristics of specific gut microbiomes linked to the therapeutic benefits of ICIs in humans.
This study is designed to elucidate the potential of the gut microbiome as a biomarker of response to ICIs using large diverse cohorts with metagenomic data and integrating it with standardized metadata.
Study design
In the current study, the researchers collected stool samples of patients aged 18 years or older who were receiving treatment with ICIs for advanced cutaneous melanoma treatment between August 2015 and January 2020. They used two separate observational prospective cohort studies: Predicting Response to Immunotherapy for Melanoma with Gut Microbiome and Metabolomics (PRIMM)-the UK and PRIMM-the Netherlands (NL), and three additional cohorts from Barcelona, Manchester, and Leeds. Data regarding baseline demographic characteristics, dietary factors, antibiotics or proton pump inhibitors (PPIs) use, tumor staging, and previous anticancer treatments were collected within three months of commencing ICI treatment.
Patients were classified as responders or non-responders based on the radiographic response. Overall response rates (ORR) and progression-free survival (PFS) at 12 months were used as clinical endpoints. Shotgun metagenomic sequencing was performed on collected stool samples. Gut microbiome taxonomy and functional profiling of metagenomes were performed using bioBakery 3.
Findings
The researchers observed a significant variation in the gut microbiome composition in the responders as compared to the non-responders in the PRIMM-UK cohort but not in the PRIMM-NL cohort. PFS12 was available for all patients in the PRIMM-NL cohort and 98% of patients in the PRIMM-UK cohort.
It was noted that in the PRIMM-UK Cohort, ORR and PFS12 were the two variables depicting the largest variance. However, in the PRIMM-NL cohort, gender, use of PPIs, Eastern Cooperative Oncology Group performance, and former antitumor regimen significantly explained the variance (potentially hiding any ORR/PFS-12-associated signatures).
While using a least absolute shrinkage and selection operator (LASSO)-based machine learning framework, the team detected a considerable gut microbiome prediction capability in PRIMM-NL when PFS12 was used as an endpoint, while in PRIMM-UK the same was observed with ORR as an endpoint. The researchers demonstrated that the gut microbiomes had a significant relationship with ICI response and were dependent on cohort type. This was owed to the characteristics of the microbial community which was related to the increased shift in the global microbiome composition.
The researchers performed an integrated analysis of different cohorts which included four previous cohorts with metagenomics sequencing data and ORR as available endpoints and two cohorts with PFS12 as available endpoints. They observed that various datasets elicited effective cohort-dependent effects in the gut microbial composition, with ‘cohort’ specifically explaining variance approximately 10 times more than any other variable.
The team confirmed that a few single data sets like the Barcelona cohort had higher ORR and PFS12 prediction levels as compared to the PRIMM-UK and PRIMM-NL, respectively. They used a setting that alleviated cohort-specific effects by taking into consideration, one cohort in the same model. The researchers observed a prediction value of 0.59 and 0.60 across ORR and PFS12 endpoints, respectively. They highlighted that functional profiling of the microbiomes resulted in increased response predictions as compared to the relative abundance in species but with high variation and reduced cross-cohort consistency.
The researchers analyzed the association of microbial taxa with ICI response across the cohorts and revealed that two Roseburia species – Roseburia sp. CAG: 182 and Roseburia sp. CAG: 471 increased in responders with ORR available endpoints across all datasets. Phascolarctobacterium succinatutens and Lactobacillus vaginalis were highly available in responders for which PFS12 data were available for seven datasets. A. muciniphila and Dorea formicigenerans exhibited 65.8% and 85.9% prevalence rates associated with ORR and PFS12, respectively. While in non-responders, Bacteroides clarus elicited higher relative abundance for both ORR and PFS12 across all seven datasets.
The team considered a panel containing texa associated with healthy host conditions. They observed that A. muciniphila had a significant association in the PRIMM-NL cohort and Ruminococcus gnavus served as a biomarker of non-responders in the PRIMM-UK cohort. No association between the response and the Blastocystis or virus presence was observed.
The researchers identified an increase in different Kyoto Encyclopedia of Genes and Genomes (KEGGS) orthologies (KOs) in responders, which included a glycosyltransferase, an increased presence of deoxyribonucleic acid (DNA) adenine methylase, and also increased gluconate symporters in non-responders.
The team found that in both PRIMM-NL and PRIMM-UK, the use of PPIs was strongly linked with microbiome composition but was not associated with PFS12 or response. In PRIMM-UK, the presence of microbiome signature is independent of PPI use. In PRIMM-UK and PRIMM-NL, 43% and 36% of individuals, respectively, experienced adverse events related to the higher immune responses. E. hallii and Anaerostipes hadrus within PRIMM-NL were associated with the absence of colitis before ICIs treatment, while in PRIMM-UK samples, no significant species emerged from the analysis. In PRIMM-UK, Bacteroides clarus was associated with ICI-induced toxicity, and in PRIMM-NL and other meta-analysis cohorts, it was associated with nonresponse. Eubacterium rectale was associated with the absence of toxicity in PRIMM-NL and with response in both PRIMM-UK and PRIMM-NL.
Conclusion
The findings of this study enhanced the current understanding of gut microbiome association with ICIs response which was cohort-dependent. This confirmed the link between microbiomes and ORRs and PFS in patients treated with ICIs.
The role of the gut microbiome is complex beyond the microbial abundance and complex interactions that existed between the microbiome and clinical and biological characteristics of patients treated with ICIs.
The authors warrant the need for further studies involving large sample sizes that consider the complex association of clinical parameters with the gut microbiome following the treatment course.
- Lee, K.A., Thomas, A.M., Bolte, L.A. et al. (2022). Cross-cohort gut microbiome associations with immune checkpoint inhibitor response in advanced melanoma. Nature Medicine. doi: https://doi.org/10.1038/s41591-022-01695-5 https://www.nature.com/articles/s41591-022-01695-5
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Adenine, Biomarker, Cell, Cell Death, Coronavirus Disease COVID-19, CTLA-4, DNA, Genes, Immunotherapy, Lactobacillus, Lymphocyte, Machine Learning, Medicine, Melanoma, Metabolomics, Metagenomics, Methylase, Microbiome, Oncology, Programmed Cell Death, Protein, Tumor, Virus

Written by
Sangeeta Paul
Sangeeta Paul is a researcher and medical writer based in Gurugram, India. Her academic background is in Pharmacy; she has a Bachelor’s in Pharmacy, a Master’s in Pharmacy (Pharmacology), and Ph.D. in Pharmacology from Banasthali Vidyapith, Rajasthan, India. She also holds a post-graduate diploma in Drug regulatory affairs from Jamia Hamdard, New Delhi, and a post-graduate diploma in Intellectual Property Rights, IGNOU, India.
Source: Read Full Article