A recent study by University of Alberta cardiologists at the Canadian VIGOUR Centre shows that a particular group of patients with stable ischemic heart disease have better outcomes with percutaneous coronary intervention (also called angioplasty with stent) or coronary artery bypass surgery and medication, versus conservative management with medication alone.
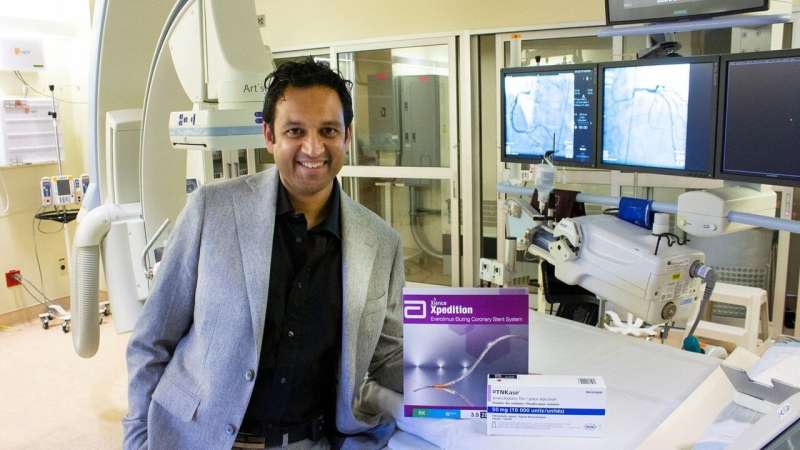
In a study published in the Journal of the American Heart Association, associate professor of medicine and academic interventional cardiologist Kevin Bainey and his team reviewed the patient information of more than 9,000 Albertans with stable ischemic heart disease. While able to function as outpatients, these patients had arteries in the heart that had narrowed and were restricting blood supply. They also had other heart issues—referred to as high-risk cardiac anatomy—including blockages in important locations of the heart’s blood vessels, or restriction in the left main artery of the heart.
The data showed that in patients with both stable ischemic heart disease and high-risk cardiac anatomy, coronary revascularization (stents or bypass surgery) led to better health outcomes, including a reduction in the risk of death or heart attack, than a more conservative approach. As well, after one year, the risk of death was 2.7 percent for patients with revascularization versus 6.8 percent for those without.
“We strongly believe coronary anatomy is an important prognostic indicator of health outcomes,” said Bainey, who is also director of the Adult Cardiac Catheterization and Interventional Cardiology Laboratory and the Interventional Cardiology Fellowship Program. “In a patient who has a higher-risk stress test and is showing symptoms, we think it’s valuable to perform a coronary angiogram to get a complete picture, rather than just managing them with medications.”
Bainey’s study builds on the landmark ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) trial, published in April 2020, which showed that in patients with stable ischemic heart disease, an invasive approach such as stents or bypass surgery did not reduce the risk of death or future coronary events in following years.
While Bainey said he agrees there is a role for conservative management in these patients, high-risk anatomy was not addressed in the ISCHEMIA trial. This prompted him to investigate further, to find out whether Alberta patients with high-risk anatomy might actually benefit from invasive approaches.
“What our results are saying is that medical management is important, but there might be a small group that would benefit from revascularization, and we need to find ways to identify that group of patients,” he said.
The results of his study also underline the importance of cardiac anatomy in determining a diagnosis and treatment options—something Bainey hopes more cardiologists will take into consideration when treating patients with stable ischemic cardiac disease.
Source: Read Full Article