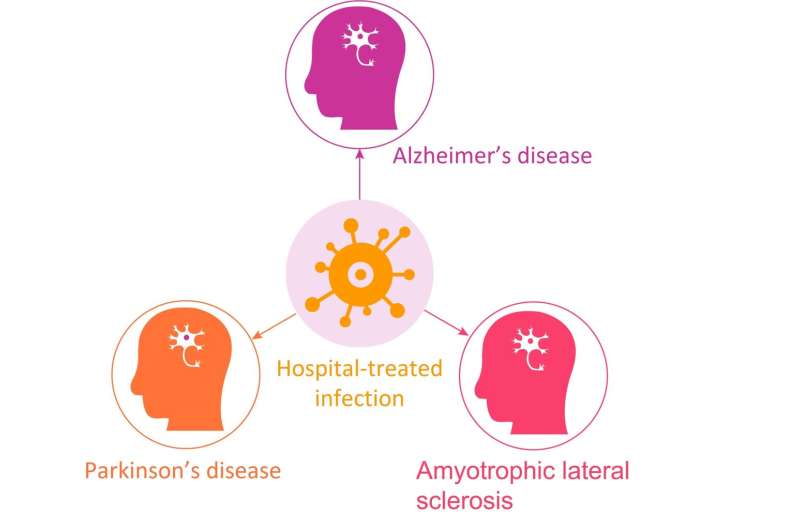
Infections treated with specialty hospital care in early- and mid-life are associated with an increased subsequent risk of Alzheimer’s (AD) and Parkinson’s diseases (PD), but not amyotrophic lateral sclerosis (ALS), according to a new study publishing September 15 in the open-access journal PLOS Medicine by Jiangwei Sun of Karolinska Institute, Sweden, and colleagues.
Experimental studies in animals have suggested that infection plays a role in the development of some neurodegenerative diseases, but supporting evidence in humans is limited. In the new study, researchers used data on people diagnosed with AD, PD or ALS from 1970–2016 in Sweden, as well as five matched controls per case, all identified from the Swedish National Patient Register. The analysis included 291,941 AD cases, 103,919 PD cases and 10,161 ALS cases.
A hospital-treated infection five or more years before diagnosis was associated with a 16% higher risk of AD (95%CI: 1.15–1.18, P < 0.001) and a 4% higher risk of PD (95%CI: 1.02–1.06, P < 0.001), with similar risks seen for bacterial, viral and other infections and for different sites of infection. The highest risk of disease was seen in people with multiple hospital-treated infections before the age of 40, with more than double the risk of AD (OR=2.62, 95%CI: 2.52–2.72, P < 0.001) and more than 40% increase in the risk of PD (OR=1.41, 95%CI: 1.29–1.53, 3 44 P < 0.001). No association was observed for ALS, regardless of age at diagnosis.
“These findings suggest that infectious events may be a trigger or amplifier of a pre-existing disease process, leading to clinical onset of neurodegenerative disease at a relatively early age,” the authors say, while also pointing out that “due to the observational nature of the study, these results do not formally prove a causal link.”
Source: Read Full Article