Obesity is now a global epidemic, and it is increasing people’s risk for cancer. The National Cancer Institute lists more than a dozen cancers that are associated with overweight and obesity. But how obesity increases cancer risk hasn’t been clear. The lab of Marsha A. Moses, Ph.D., at Boston Children’s Hospital, now draws a direct link—one with possible implications for cancer screening and treatment.
Their study is published in the journal Proceedings of the National Academy of Sciences.
Focusing on one common cancer, breast cancer after menopause, Moses and her team provide compelling evidence that obesity may cause previously dormant tumors to trigger the formation of new blood vessels, a process called angiogenesis or neovascularization. Once nourished with a blood supply, the tumors grow and become more of a threat.
The team then showed, in mice, that giving a drug to inhibit blood vessel formation kept breast tumors in their dormant state.
“We know that once blood vessels invade a tumor, the tumor can begin to grow exponentially,” says Moses, who directs the Vascular Biology Program at Boston Children’s. “If we can delay tumors from escaping dormancy or from growing early on, they would be less challenging to treat.”
Watching tumors escape dormancy
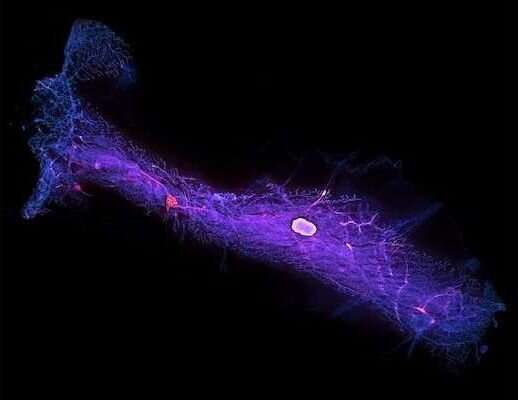
Led by Roopali Roy, Ph.D., the researchers created a complex model involving obese menopausal mice that would allow them to observe tumor neovascularization in real time. They then injected human breast tumor cells, bearing an enzyme called luciferase, into the mammary fat pads of both obese and lean mice.
Finally, to detect the invasion of new blood vessels into the tumors, they injected another compound, luciferin, into the animals’ bloodstreams. When luciferase and luciferin meet, they light up as a bioluminescent signal, indicating that blood vessels have reached the tumor.
The team then tracked subsequent tumor growth through a series of imaging studies.
Initially, the tumors did not light up because no blood vessels (and hence no luciferin) reached them. But within three to six weeks, blood vessels began invading the tumors of the obese mice, which lit up dramatically. In contrast, tumors in the non-obese mice were still dormant at 12 weeks.
Signals from fat cells
Probing further in the lab, Roy and her colleagues found that fat cells from the obese mice were secreting higher levels of compounds that promote angiogenesis: lipocalin-2, vascular endothelial growth factor, and basic fibroblast growth factor. These apparently enabled the tumors to come out of dormancy and start progressing.
“With obesity, fat cells grow very large, and as this happens, they become more oxygen-starved and begin to die through apoptosis, which often leads to inflammation,” explains Roy. “This causes the fat cells to secrete angiogenic factors to bring in more blood vessels and increase oxygen delivery. If there’s a dormant tumor in the tissue, it is now surrounded by this inflammatory, angiogenic microenvironment and can switch on.”
When the obese mice received sunitinib, a drug that inhibits blood vessel formation, tumor latency was prolonged and tumor-free survival increased. The lab has now shown in multiple mouse models that such inhibitors can maintain breast tumors in their dormant state.
Obesity and cancer biomarkers in urine
The Moses Lab now wants to translate these findings to postmenopausal women with breast cancer, tapping its well-known urine biorepository. The lab’s vision is to screen obese or overweight women for breast cancer by testing their urine for biomarkers indicating that a tumor has become vascularized and has begun growing—even before it is palpable.
Women testing positive could potentially be treated with an inhibitor of blood vessel formation or other targeted drugs to keep their cancer dormant or at least slow it down, says Moses. Her team has already identified a panel of urinary biomarkers and is validating their utility across different cancer types, including breast cancer.
In a related investigation, the team is comparing women’s urine samples before and after bariatric surgery for obesity to see whether biomarkers change after the surgery. If any of the women develop breast cancer, the team can look for markers in their earlier urine samples that could have predicted the cancer.
Analyzing fat tissue
The researchers are also exploring how fat tissue changes in the context of cancer via a first-of-its-kind biorepository of adipocytes (fat cells) from pre- and postmenopausal women. Partnering with breast surgeon Susan Pories, MD, and Meg Lotz, Ph.D., at Mount Auburn Hospital and the Beth Israel Deaconess Medical Center, they have obtained adipose (fat) tissue surrounding breast tumors that had been surgically removed. For comparison, they obtained breast fat tissue from healthy women who had breast reduction surgery.
“We can use RNA sequencing and other approaches to look for differences in which genes are turned on and off, and proteomics to see what factors the tissue is secreting,” says Roy. “We then can test these factors to see how they affect tumor cells. Once we have a list of targets, we can try knocking them out, in a dish and in live mice, to see if that affects tumor progression.”
Through these and other resources, the lab’s ultimate goal is to gain insights into obesity-related cancers in general.
“The association between obesity and a number of cancers is finally being appreciated,” Moses says. “We have an opportunity to identify the mechanisms underlying these associations and leverage them to develop therapeutics and diagnostics for these special types of cancer.”
More information:
Roopali Roy et al, Escape from breast tumor dormancy: The convergence of obesity and menopause, Proceedings of the National Academy of Sciences (2022). DOI: 10.1073/pnas.2204758119
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article