After the start of the SARS-C0V-2 pandemic, investigators from ResearchPath LLC and their collaborators at Rutgers University quickly dedicated resources to develop accurate and reliable COVID-19 testing. As variants emerged, they developed a PCR test that uses molecular beacons not only to diagnose COVID-19 infection, but also to identify the specific variant causing that infection. Their research appears in The Journal of Molecular Diagnostics. Their methodology is openly available so that it can be replicated by any facility that can run a PCR test.
“It is extraordinary to see that SARS-CoV-2 was not a monolithic infection with a predictable set of clinical features, but rather an ever-evolving disease for which the different strains produce unique clinical features that affect testing, symptoms, and even which organ systems can be attacked,” explained lead investigator Sanjay Tyagi, Ph.D., Public Health Research Institute, New Jersey Medical School, Rutgers University, Newark, NJ, U.S..
Identifying specific strains reveals important information such as the length of incubation period, length of contagious period, transmissibility, pathogenicity, and even changes in the predominant symptoms.
Information on strain types is generally reported by the international community or a few states with large populations that perform genetic sequencing. The deep sequencing needed to identify SARS-CoV-2 strains is accurate and can identify each mutation present in a sample, but it is costly, slow and requires specialized equipment. Yet knowledge of the strain type provides important information for public health professionals, policymakers, and individuals.
“Knowing that a highly contagious and dangerous strain is emerging in a local community could inform policymakers to initiate safety measures to limit spread,” said co-investigator Ashley Hill, MD, ResourcePath LLC, Sterling, VA, U.S.. “It can also serve as an early warning system for healthcare systems that need to plan for surges in ER visits and ICU care. Knowing which strain has infected a person can also help determine which treatments would be most beneficial.”
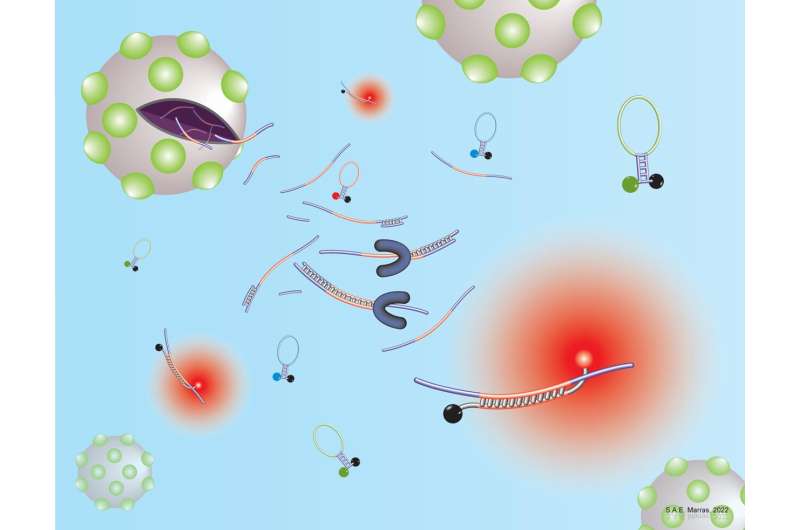
Using real-time PCR probes designed by Rutgers University and already used around the world for many purposes, Rutgers designed the Rutgers-RP RT-PCR assay to detect mutations in SARS-CoV-2 that have been shown to increase immune escape, avoid neutralization, and increase transmissibility. They pioneered the use of molecular beacons to identify specific genetic mutations. Molecular beacons are hairpin-shaped molecules that can be designed to selectively bind to a specific mutant sequence, avoiding wild-type sequences that often differ by a single nucleotide.
Nine mutations were selected for testing, and the beacon for each has differently colored dyes. Every original variant of concern—Alpha, Beta, Gamma, Delta, and Omicron—has a unique combination of these mutations. and when the beacon binds to its target molecule, its distinct color can be detected by the assay.
Each beacon was tested individually to confirm its specificity to the assigned mutation. Then, the beacons were combined into a multiplex assay and tested by RT-PCR on 26 SARS-CoV2–positive patient samples that had previously been tested and identified with deep sequencing. Two samples were identified as the Alpha variant, two as the Epsilon variant, and eight as the Delta variant. The multiplex assay was in full agreement with results from deep sequencing, with a sensitivity and specificity of 100%.
Researchers report that the test is also very adaptable. When Omicron emerged, the investigators were able to design a beacon in less than a month to identify a mutation that is unique to Omicron and is important for immune evasion. The investigators identified the Omicron variant in 17 of 33 additional patient samples that had been previously tested, and the results were 100% in agreement.
“The tools we developed to track and identify new variants will be useful for this pandemic and for any unforeseen viruses or pathogens that may arise going forward,” said lead author Ryan J. Dikdan, BS, Public Health Research Institute, New Jersey Medical School, Rutgers University, Newark, NJ, U.S..
Source: Read Full Article