
Covid Heads Towards Another Winter
Paul Gigot interviews Dr. Marty Makary
Katrina Haydon can’t eat, shower or brush her teeth the same way she used to six months ago because of parosmia, a smell disorder sometimes associated with COVID-19 “long-haulers,” or people whose COVID symptoms last long after they test positive for the virus.
Parosmia
Parosmia is a term used for any kind of distortion of one’s sense of smell — unlike anosmia, a term for one’s loss of their sense of smell.
For Haydon, 24, it started with anosmia. She believes she contracted COVID-19 in June of 2021, though she tested negative for the virus. She had mild cold-like symptoms and lost her sense of taste and smell, as many COVID patients do. The anosmia lasted for several weeks before about 70% to 80% of her taste and smell senses returned.

A healthcare worker inserts a Covid-19 rapid test into a machine at the CareNow Denver University urgent care center in Denver, Colorado, U.S., on Tuesday, Nov. 16, 2021. Photographer: Daniel Brenner/Bloomberg
Then, in September, the parosmia symptoms kicked in.
“Savory foods smell like rotting sewage. Hot water smells like rotting meat. Chemical cleaner and perfume smell like really sharp, overwhelming sulfur — like the smell of hair burning but concentrated and stronger. Sweets and dairy taste like perfume would taste if you sprayed it in your mouth,” she told Fox News.
Haydon’s aversion to the smell of heat — such as the smell of a hot shower or radiator — is perhaps the strangest aspect of her condition.
“I used to take a shower more than twice a day regularly, but at least twice a day, and it has been really, really hard for me to make myself shower once a day. It’s so difficult,” she said. “And same thing with brushing my teeth. It’s really, really hard because even non-mint toothpastes cause a physical reaction because they just taste and smell so bad.”

Workers assemble a heater in an outdoor dining area at a restaurant in San Francisco, California, U.S., on Wednesday, Aug. 5, 2020. Photographer: David Paul Morris/Bloomberg
(Photographer: David Paul Morris/Bloomberg via Getty)
The experience has been isolating and even depressing.
If her neighbors cook, it smells bad. Public transportation smells bad (or at least worse than normal). CVS and Whole Foods smell bad. Restaurants smell terrible. It has driven her away from seeing friends in social settings.
“I think everybody believes me, but I don’t think they realize — I think a lot of people don’t realize — the severity of it,” Haydon said. “It seems like, oh, everything smells and tastes bad, that stinks, but I don’t think the extent to which it does change your day-to-day life is immediately evident to most people. I think it takes a little time to understand what that really does look like.”
How does it happen?
Dr. Andrew Lane, Director of the Sinus Center at Johns Hopkins and professor of otolaryngology — head and neck surgery — at Johns Hopkins School of Medicine, told Fox News that parosmia not only appears in some COVID-19 survivors, but it can also occur after people catch other viral infections or suffer brain injuries, brain tumors and Multiple Sclerosis.
Lane, who is studying the phenomenon in COVID-19 survivors, says it all starts in membranes located in the upper part of a person’s nose.
“Your whole nose is lined with mucous membranes … and in the upper part of the nose, there’s this very specialized mucous membrane, and that’s where you sense smells. And this is really a unique kind of tissue in the body,” he said. “First of all, it’s the only place in the body where a neuron that’s coming from the brain directly contacts the outside world … and the part that sticks out in the environment can is what actually can detect an [odor molecule]. … And then and then it sends a signal like straight to the brain.”
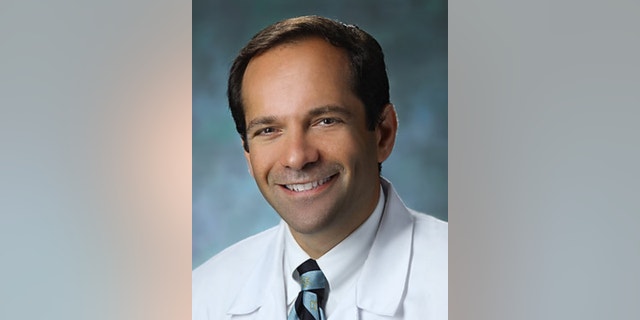
Dr. Andrew Lane (Johns Hopkins School of Medicine)
That unique tissue is called the olfactory epithelium. The membranes in that part of the nose remember what certain objects are supposed to smell like.
But with anosmia and parosmia, those neurons, which are supposed to send signals to the brain after encountering an odor molecule and inform the brain of what it is, get lost along the way.
“COVID has this ability to infect the olfactory tissue and the olfactory epithelium … and you lose a lot of neurons, sort of all at once. And if you lose a lot of it, you know, maybe all of it, then you’re going to be anosmic,” Lane explained, adding that it’s “not exactly clear how this happens.”
His recent study shows that COVID-19 cells, which latch onto and infect olfactory cells, are 700 times more prevalent in the upper part of the nose that send odor signals to the brain than they are in “the lining cells of the rest of the nose and windpipe that leads to the lungs.”
Usually, a person’s sense of smell returns quickly after contracting COVID-19, but sometimes it can take months; in rare cases, people can lose their smell indefinitely.

Three days after testing positive for Covid-19, "everything tasted like cardboard," recalls 38-year-old Elizabeth Medina, who lost her sense of taste and smell at the start of the pandemic. (Photo by ANGELA WEISS/AFP via Getty Images)
When a person experiences anosmia, sometimes they can gain their sense of smell back by smelling potent foods, like grapefruit, because the brain can remember how those foods are supposed to smell.
But with parosmia, neurons send the “wrong” signals to the brain, which is why Haydon and others can’t eat or walk into restaurants — because everything smells too awful.
Lane says as devastating as this is for most people who experience it, it’s actually a good sign.
“That means that it’s coming,” the professor said, “it” meaning an accurate sense of smell. “It’s starting to work again, and that there may be some sorting out to do, but at least the elements are finding their way back together, getting to your brain, getting some signal when your nose is getting a smell, which is better than nothing. … The brain sorts it out, and over time, you get your sense of smell back.”
How is it treated?
Haydon has turned to online forums, TikTok, YouTube and Twitter to find answers because doctors haven’t given her much to work with.
There are a mix of people experiencing the issue: young people, older people, men, women, vaccinated, unvaccinated. Many say they experienced mild COVID-19 symptoms before suddenly experiencing parosmia weeks or months after contracting the virus. She’s read about parents who can’t cook for their families anymore or sit with them at the dinner table.
Yet for such a debilitating issue for potentially thousands of people, if not millions, globally, there is no confirmed solution.

Leah Holzel, 60, a food editor who had lost her sense of smell from 2016 to 2019, now coaches people who have lost their sense of smell due to Covid-19. (Photo by ANGELA WEISS/AFP via Getty Images)
Haydon has read about solutions ranging from alpha-lipoic, an antioxidant found naturally in human cells, to IV drips, zinc and even chiropractic methods.
“It’s pretty varied,” she said. “Mostly, it’s people saying, ‘Have you tried this? Have you tried this?’ But most of the people I see that say, ‘Oh, I did this, and it worked,’ is the alpha-lipoic.”
Lane said he’s heard of using alpha-lipoic acid as a solution, but “there’s not very good evidence that [it] works.”
“I mean, there’s a whole industry of different things that people give to people with olfactory loss, and mostly it’s snake oil kind of stuff, and there’s very kind of skimpy data about it,” he said. “But there is no medication that we have that restores a sense of smell.”
Ultimately, COVID-19 is too new. It’s only been around for about two years, so “long” COVID symptoms and long-term effects of the virus are still largely unknown.
Most of the patients Lane sees who can’t taste food or experience a bad reaction to the smell of food have to force themselves to eat because they know they’re hungry even though the act of eating seems unappealing.
“It’s a frustrating problem that we don’t have a treatment for,” he explained. “And I think we’re going to see more and more patients with this problem. The answer, ultimately, is going to be research. … We’ve been interested in this kind of general problem of how the sense of smell works and what can go wrong. But I think that ultimately the way out of this is to understand better and how the system works and develop treatments.”
Source: Read Full Article