Mutations in a gene related to HER2, a gene frequently implicated in breast cancers and a variety of other malignancies, can amplify activity that spurs tumor growth, a new study led by UT Southwestern researchers suggests. The findings, published online in Cancer Cell, could explain why many patients with HER2 mutations don’t respond to inhibitors that target this cancer driver and require other treatment.
“Within the precision oncology field, we typically focus on targeting one mutant gene with one drug,” says study leader Ariella B. Hanker, Ph.D., assistant professor of internal medicine and Harold C. Simmons Comprehensive Cancer Center member. “This study showed that in some patients you might have to look at more than one mutant gene to find the best drug or combination of treatments.”
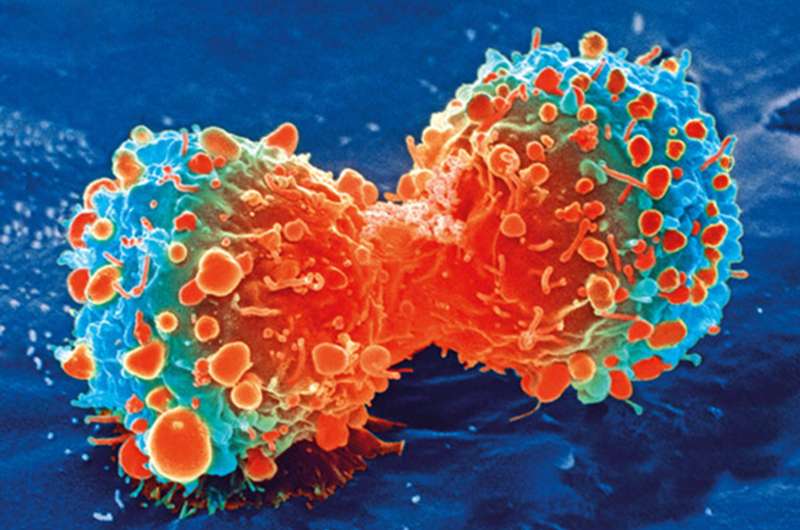
For decades, researchers have studied the role of HER2 in breast cancer and other cancer types. The protein produced by this gene is a growth factor receptor that when activated stimulates cells to divide. In about 25 percent of breast cancers, tumor cells carry extra copies of this gene, causing too much of the protein to be made and leading cells to divide continuously—a hallmark of cancer. Because this aberration is so common, checking for its presence is typically a standard part of breast cancer diagnostics.
Recent research has suggested that in about 5 percent of advanced breast cancers, the HER2 gene is mutated in a way that activates it, mimicking the effects of carrying extra copies, Hanker explains. Clinical trials have found that cancer drugs that inhibit the mutant HER2 protein can successfully shrink tumors. However, patients with additional mutations in a related gene called HER3 were resistant to these treatments.
To better understand this phenomenon, Hanker, along with study co-leader Carlos L. Arteaga, M.D., professor of internal medicine and director of the Simmons Cancer Center, and their colleagues investigated how mutated HER2 and HER3 proteins interact.
Computer modeling showed that mutations in both genes caused the resulting proteins to bind together more strongly than their nonmutant forms, even without a helper molecule that’s usually necessary for these proteins to work together. These modeled predictions held true when the scientists mixed different HER2 and HER3 proteins in the lab.
When the researchers mutated only HER2 in healthy breast cells, they grew in round balls, a key characteristic of tumors. But when they also mutated HER3, these balls grew spikes that invaded the surrounding matrix, an important step toward metastasis.
Additional computer modeling showed that the tight binding between the mutant HER2 and HER3 proteins prevented HER2-inhibiting drugs from attaching to the HER2 protein, hampering their effectiveness. When the researchers added a second drug that indirectly inhibits HER3, cancer cells that carried both mutations died.
“Patients that carry both HER2 and HER3 mutations are likely not going to be good candidates for treatments by HER2 inhibitors themselves,” Hanker says. “By also inhibiting the action of HER3, we can make some headway against these tumors.”
Source: Read Full Article