Genetic testing and counseling for inherited cardiovascular diseases may help patients and their families make well-informed decisions about managing their heart health, according to “Genetic Testing for Inherited Cardiovascular Diseases,” a new scientific statement from the American Heart Association, published today in the Association’s journal Circulation: Genomic and Precision Medicine.
The statement summarizes what we know—and do not know—about the genes or combination of genes that may influence inherited heart diseases and also provides suggestions for best practices for genetic testing.
“Although genetic testing has seen explosive growth in the past few years, both in the clinical setting and with direct-to-consumer testing, genetic testing for heart disease should be reserved for specific patients,” said Kiran Musunuru, M.D., Ph.D., M.P.H., M.L., FAHA, chair of the writing group for the scientific statement and professor of cardiovascular medicine and genetics at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
According to the statement, cardiovascular conditions that may have an inherited genetic component include:
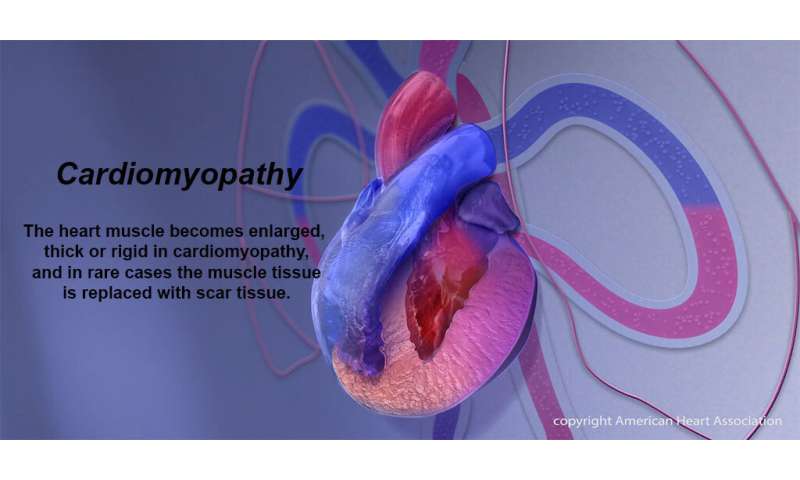
- cardiomyopathies, heart muscle diseases that can lead to heart failure;
- thoracic aortic aneurysms and dissections, syndromes that cause the body’s major artery to balloon and rupture;
- arrhythmic disorders that predispose people to potentially fatal abnormal heart rhythms; and
- familial hypercholesterolemia, or highly LDL elevated cholesterol levels that greatly increase the risk of heart attack.
Before considering genetic testing, a health care provider should work with the patient to document their family medical history, ideally, going back three generations, to determine if there is a pattern of certain types of heart disease. Genetic testing should typically be reserved for patients with a confirmed or suspected diagnosis of an inherited cardiovascular disease or for individuals at high risk due to a previously identified disease-causing variant (a gene abnormality that is different from most humans, often responsible for the clinical disease in question) in their family.
Genetic counseling is essential before genetic testing to educate patients on the process and potential results, as well as the potential risks and uncertainties related to testing. Counseling is also critical after genetic testing, so the counselor can explain the results and potential consequences for the patient’s health and the health of family members including children.
Since immediate family members—first-degree relatives such as fathers, mothers, siblings or children—might share genetic variants predisposing them to an inherited cardiovascular disease, they are considered to be at higher risk for the same conditions. Once a genetic variant is identified within a family, all first-degree relatives should consider undergoing genetic testing and counseling for that specific mutation whenever possible.
Genetic counselors can also advise and support patients on the best ways to communicate the news of any genetic variants they may discover through genetic testing to other family members. Although privacy laws restrict the ability of health care professionals to disseminate information directly to potentially affected relatives, they can provide written letters that explain the genetic findings, which the patients can give to their family members.
“With most genetic cardiovascular diseases, inheriting a mutation (or variant) from a parent substantially increases the risk of getting the disease but does not guarantee the disease,” said Musunuru. “In some cases, it might be possible to act early and prevent the disease. In other cases, having the mutation for a genetically caused cardiovascular condition might lead to different and possibly more aggressive treatment.”
Advances in human genetics are improving the understanding of a variety of inherited cardiovascular diseases. However, there are still limitations. Genetic testing might not reveal a cause or confirm a diagnosis of the patient’s disease.
In many cases, genetic testing can reveal a mutation that is called “uninterpretable” or a “variant of uncertain significance.” A variant of uncertain significance, or VUS, is not considered either definitively pathogenic (disease causing) or benign, meaning that it’s unclear if the patient is at increased risk for disease. Since it is unclear whether the VUS increases the risk of disease or not, it can be challenging for doctors to counsel patients on appropriate treatment.
It is also possible that a patient may be diagnosed with an inherited cardiovascular disease, yet genetic testing doesn’t reveal any genetic mutations. This makes it difficult to explain why the patient has the disease and whether any of their family members are also at risk.
Source: Read Full Article