Many scientists working on diseases affecting people in developing countries and their animals are refocusing part of their work on COVID-19. The result is that while the pandemic response is receiving a welcome boost, the prospect for research into lesser-known diseases of poor people in poor countries is less certain.
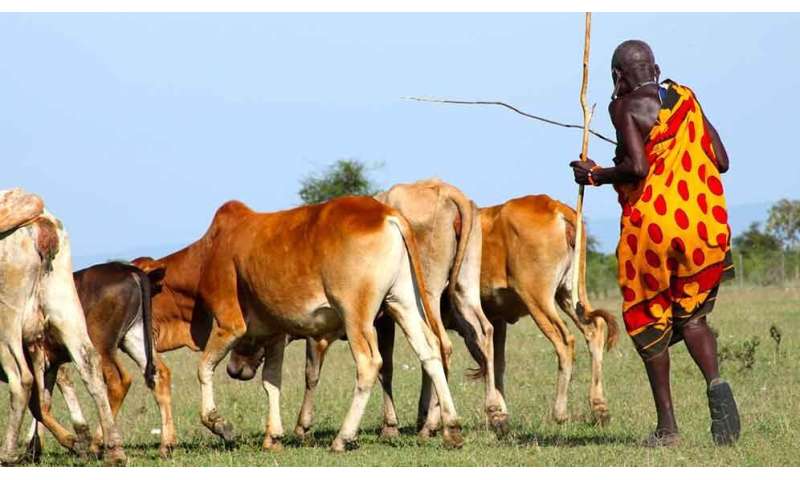
Most diseases that transmit from animals to humans (zoonoses) are not of the headline-grabbing, world-stopping variety. They are an everyday reality for millions of people whose lives are quietly blighted or prematurely ended by diseases transmitted through farming and food systems.
These include trypanosomiasis, which impacts livelihoods when cattle are infected and in people causes sleeping sickness, and non-typhoidal salmonella, which in Sub-Saharan Africa alone kills an estimated 100,000 people a year.
Scientists in Africa, Asia and Europe from a range of disciplines have been researching these diseases of poverty as part of Zoonoses and Emerging Livestock Systems (ZELS), a United Kingdom Department for International Development (DFID) and UK Research and Innovation funded programme. Their expertise has new and critical relevance to the COVID-19 outbreak.
Repurposing knowledge
While the crisis has, for example, brought to a halt routine bench work in the avian influenza lab at the Pirbright Institute, where Munir Iqbal has led a ZELS team researching bird flu vaccines for poultry flocks in Asia, the team’s work is now helping to understand the biology and transmission of COVID-19.
Other ‘redeployment’ includes that of medical anthropologist Hayley MacGregor, who has been studying the social relationships behind foodborne diseases transmitted from pigs to people in Myanmar. She is now advising the World Health Organization (WHO) on incorporating social science approaches into the global COVID-19 response.
The diagnostic laboratory at the International Livestock Research Institute (ILRI) in Nairobi, where the ZooLinK project is doing surveillance for 15 different zoonotic pathogens, has been turned in to a COVID-19 testing centre supporting the Ministry of Health. Several project staff are contributing to testing, with others engaged in contact tracing COVID-19 cases.
In ZELS-supported facilities in Pakistan, Tanzania, Ethiopia and elsewhere, the well-equipped laboratories with local ZELS-trained staff are now contributing to national coronavirus testing and surveillance efforts.
One Health
As a result of the UK investment in rigorous, interdisciplinary ‘One Health’ science, a global network of scientists is now better placed to work on today’s coronavirus pandemic.
One Health recognises that human, animal and environmental health are inter-connected. A collaborative, interdisciplinary and integrated approach to zoonoses research, policy and management is needed.
But what now for people affected by those less newsworthy endemic zoonoses—the zoonotic infections that millions of people live with every day and that are not being monitored by the whole world—and that circulate in the farming and food supply systems?
We know that people in developing countries are often less able to deal with health threats, not just as a consequence of weaker health systems, but also because diseases compound each other and poverty compounds the impacts of infectious disease.
It is also almost inevitable that endemic diseases will stop getting the attention they need as health systems gear totally towards the crisis. This was seen in West Africa during and after the Ebola outbreak in 2014.
This pandemic will bring changes to human behaviours that could lead to changes in other zoonotic disease risks.
A key outcome from the ZELS work on viral and bacterial zoonoses with pastoralists in Tanzania was recognition of the importance of handwashing and biosecurity measures for reducing the risk of transmission. Given the numerous challenges in implementing livestock vaccination, handwashing advice disseminated to prevent the spread of COVID-19 could lead to a reduction in transmission of other zoonoses.
Endemic diseases are not going away. Fortunately, ZELS research is now starting to have impact.
Managing zoonoses
A finding that treating cattle with insecticides to combat ticks and tsetse flies can contain the risk of sleeping sickness in people offers the possibility of simple and cost-effective disease-management strategies.
Discovering that the majority of schistosomiasis transmission and sickness in Senegal and Niger is driven not by a human schistosome species, as had been previously assumed, but through schistosome species from people and their livestock combining to form highly transmissible viable parasitic hybrids, has helped ensure the WHO embraces a One Health approach to eliminating of a disease that infects more than 240 million people globally.
National strategies for brucellosis in Kenya and Tanzania, bovine tuberculosis in Ethiopia and avian influenza in Bangladesh are now being influenced by ZELS findings. ZELS work around the social and cultural contexts in which disease risks emerge is feeding into critical risk mitigation measures.
This important science needs to continue. The ZELS projects have inevitably had to call a halt to their field- and lab-based work, and their policy partners are largely and understandably focused on the current public health emergency.
Source: Read Full Article