The COVID-19 pandemic has profoundly affected cancer diagnoses and treatments. Colonoscopies, for instance, have decreased 90% in the past year. While screenings are down, experts say that the number of young people developing colorectal cancer before 50 continues to increase. This trend began in the early 1990s.
“The majority of those increases are in people ages 40 to 49, but half of young-onset colorectal cancer patients are under 40 years old,” says Dr. Lisa Boardman, a Mayo Clinic gastroenterologist. “We used to think of colorectal cancer as a disease of aging. With the increase in the number of cases of colorectal cancer globally, there are clearly other factors in addition to aging that contribute to the development of colorectal cancer.”
But why are people developing colorectal cancer at a younger age?
“It’s not accounted for by a known hereditary condition. About 20% of the people who develop early-onset or young-onset colon cancer will be found to have a hereditary type of genetic change. The majority of them do not,” says Dr. Boardman. “Possible explanations may be related to changes in diet, increasing rates of obesity and decreased physical activity, but at this point, why more younger people are being diagnosed with colorectal cancer remains unknown.”
The goal of screening for colorectal cancer and precancerous polyps that may develop cancer is to identify cancer at an earlier, and more likely curable, stage. Dr. Boardman says, “Then precancerous colorectal polyps can be identified and removed through polypectomy, thereby preventing colorectal cancer. Screening means that this testing is done before a person develops any signs or symptoms that may be caused by having a cancer or polyp.”
The U.S. Preventive Services Task Force recommends screening beginning at 50. Earlier screening is recommended for some groups, depending on risk factors. African Americans, for instance, have an increased risk of developing colorectal cancer and are encouraged to begin screening at 45.
Because most younger people will not be screened, it is especially important to be aware that symptoms can include abdominal pain, change in normal bowel pattern, unexplained or unintended weight loss, blood in the stool or dark tarry stools. Fatigue can result from blood leaking from the tumor and leading to anemia, a decrease in oxygen-carrying hemoglobin that is measured by a blood test.
Risk factors include:
- Family history.
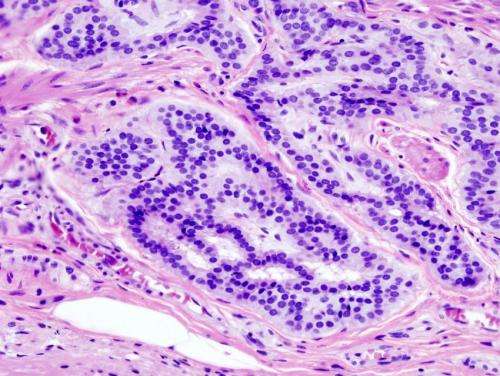
- Inflammatory bowel disease.
- Diabetes.
- Low-fiber and high-fat diet.
- Radiation therapy for cancer.
- Hereditary colon cancer syndrome.
Dr. Boardman says knowing your family health history is important. “If a patient has a family history of colon cancer, it can help with the type of screening we perform. We’re looking for conditions, and the most common hereditary issue is called Lynch syndrome,” says Dr. Boardman. People who have Lynch syndrome have an inherited mutation in a gene that increases your risk of colon cancer, endometrial cancer and several other cancers involving the colon.
Diet and exercise can help prevent colorectal cancer, and contribute to overall good health.”We know focusing our diets more on fruits and vegetables, minimizing the amount of red meat and processed meats like bacon and sausage that have nitrites in them, along with reducing alcohol intake, avoiding tobacco and increasing physical activity can have an impact on our overall health,” says Dr. Boardman.
Source: Read Full Article