Stem cell-based therapy improved quality of life for patients with advanced heart failure, Mayo Clinic researchers and international collaborators discovered in a late-stage multinational clinical trial. In one of the largest studies of cell intervention after a heart attack, patients reported their daily hardship lessened when stem cells optimized for heart repair supplemented the standard of care.
This clinical study further documented lower death and hospitalization rates among those treated with cell therapy. This research is published in Stem Cells Translational Medicine.
“In this era of global aging, people live longer, yet are at risk of chronic disease imposing a poor quality of life. Heart failure is an emerging epidemic in need of new healing options,” says Andre Terzic, M.D., Ph.D., a Mayo Clinic cardiovascular researcher and lead author of the paper.
“The stem cell-based approach in the present study demonstrates sustained benefit on physical and emotional health in response to biotherapy.” Dr. Terzic is the Marriott Family Director, Comprehensive Cardiac Regenerative Medicine for the Center for Regenerative Biotherapeutics.
Approximately 800,000 people in the U.S. suffer heart attacks every year. Damage to cardiac muscle weakens the heart’s ability to pump blood through the body, leading to heart failure—a debilitating and life-threatening disease.
People with heart failure often suffer a diminished quality of life associated with shortness of breath, fatigue, swollen legs, and limited daily activities. The standard of care for heart failure includes a heart-healthy diet and habits, medications, implantable devices, and rehabilitation. However, current regimens do not work for everyone, especially in advanced disease stages.
The research
The study team recruited 315 patients from 39 hospitals in 10 countries who had advanced heart failure despite receiving standard care. Patients were randomly divided into groups that would receive stem cell therapy versus those who would not. Patients assigned to cell treatment underwent cardiac catheterization.
Then, stem cells taken from their own bone marrow and programmed to heal damaged heart tissue were delivered to the heart. Patients assigned not to receive stem cells had cardiac catheterization without cell delivery—known as the sham treatment.
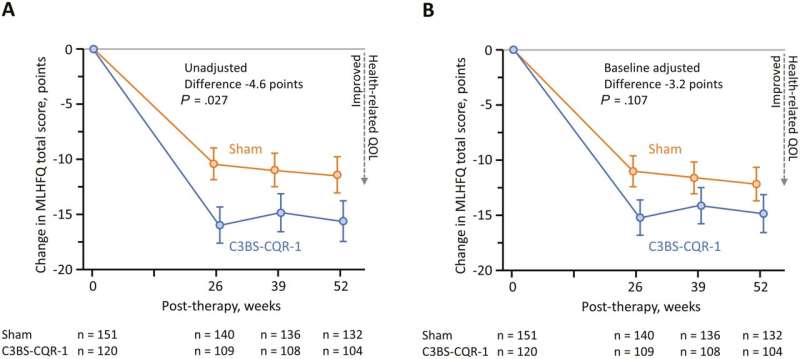
All participants were asked to complete a 21-question self-assessment at the beginning of the study and then again at 26-, 39- and 52 weeks following treatment. For each question, they rated their physical, behavioral, and emotional states on a scale of 0 to 5.
During the one-year follow-up, patients with preexisting left cardiac chamber enlargement consistently reported improved quality of life after cell therapy over those who received the sham treatment. In parallel, lower death and hospitalization rates were recorded among those who received stem cells.
“Data from one of the largest cardiovascular cell therapy trials, testing a regenerative technology discovered at Mayo Clinic, indicate benefit in both quantity and quality of life in advanced heart disease,” says Satsuki Yamada, M.D., Ph.D., a Mayo Clinic cardiovascular researcher, and first author on the study. “The benefit of regenerative care has been typically evaluated on the basis of clinician-reported outcomes. What’s unique in this study is that it was designed to listen to the patient’s experience.”
This clinical trial was conducted in a double-blinded fashion, with both participants and their health care professionals masked during the study assignment. A double-blind study is designed to reduce the risk of bias when evaluating patient outcomes.
More information:
Satsuki Yamada et al, Cell Therapy Improves Quality-of-Life in Heart Failure: Outcomes From a Phase III Clinical Trial, Stem Cells Translational Medicine (2023). DOI: 10.1093/stcltm/szad078
Journal information:
Stem Cells Translational Medicine
Source: Read Full Article