The immune-modulatory effect of lenvatinib investigated in new study
New drugs are being developed and used to combat a variety of malignancies. Among these is lenvatinib, an antagonist of multiple growth factors, including vascular endothelial growth factor receptor (VEGFR) 1-3, fibroblast growth factor receptor (FGFR) 1-4, and platelet derived growth factor receptor alpha, which allows this agent to inhibit angiogenesis and cell proliferation.
Lenvatinib is currently used to treat differentiated thyroid carcinoma (DTC) which is refractory to radioactive iodine (RAI). A new study published in Scientific Reports explores the effect of lenvatinib treatment on patients with advanced thyroid cancer.
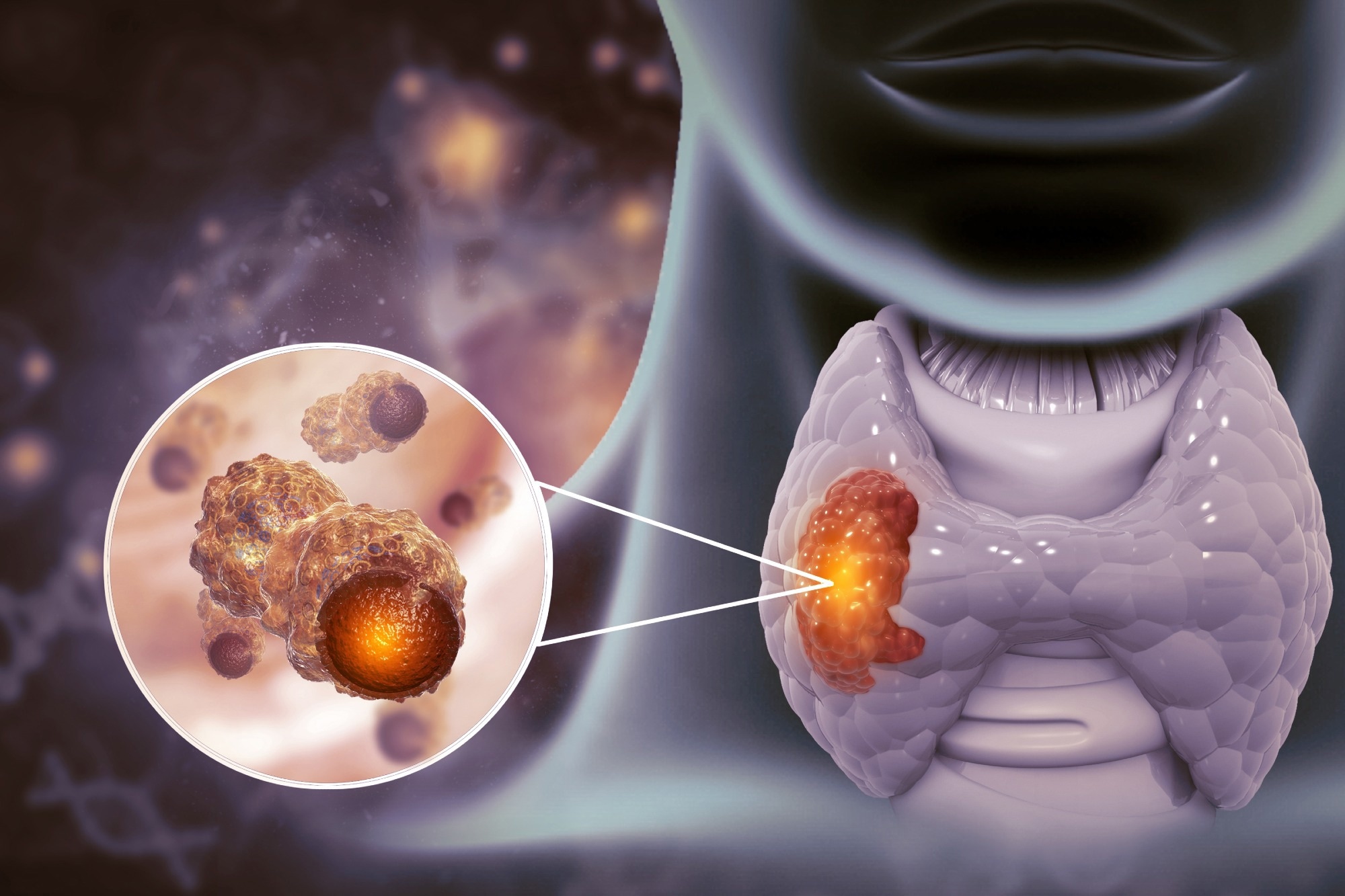 Study: Changes in peripheral blood immune cell population in thyroid cancer patients treated with lenvatinib. Image Credit: crystal light / Shutterstock.com
Study: Changes in peripheral blood immune cell population in thyroid cancer patients treated with lenvatinib. Image Credit: crystal light / Shutterstock.com
Introduction
Lenvatinib is associated with superior real-world efficacy against RAI-refractory DTC, perhaps because it blocks both FGFR and VEGFR. This prevents the emergence of resistance to this agent, thereby prolonging its duration of efficacy.
Lenvatinib also has a possible immunomodulatory effect, which is currently being evaluated in preclinical studies. These immunomodulatory effects include better tumor infiltration, natural killer (NK) cell activation, and reduced tumor-associated macrophages. NK cells are central to the innate immune antitumor response, as they mediate the natural cytotoxic reaction to tumor cells, thereby inhibiting their growth and spread.
The current study sought to confirm this activity of lenvatinib using peripheral blood mononuclear cell (PBMC) profiles as a marker of host immunity in lieu of tumor-infiltrating immune cell measurements. To this end, the peripheral immune cell profile was compared between two and four times for each patient at two to three month intervals using the Maxpar Direct Immune Profiling Assay.
A total of ten patients were included in the current study, with a mean of three samples obtained from each patient. The median age of the patients was 65 years.
What did the study show?
All patients responded well to lenvatinib, which showed a durable effect. The major difference between the PBMC profiles when pre-treatment, on-treatment, and off-treatment samples were compared was the proportion of NK cells.
Among total live PBMCs, NK cells accounted for 9% before treatment and subsequently rose to about 21% in on-treatment samples, the latter of which comprised both early and late NK cells. In off-treatment samples, NK cell levels declined to 13%, with a significant reduction in early NK cells in this group.
Following treatment, the total NK cell proportion also rose significantly in the CD45 cell subgroup from about 10% to 19%. There were no significant changes in monocyte proportions or the lymphocyte-to-monocyte ratio (LMR).
The assessed cytokines included interleukin 2 (IL-2) and IL-15 among the NK cell activators, as well as IL-10 and transforming growth factor β (TGFβ) among NK cell inhibitors, all of which did not change significantly following treatment.
What are the implications?
Our results present the immune-modulatory effect of lenvatinib in a real-world clinical setting.”
Taken together, the study findings demonstrate that NK cell populations significantly increased in thyroid cancer patients treated with lenvatinib.
These findings corroborate earlier research conducted in hepatocellular carcinoma mouse models, in which immunocompetent mice responded to lenvatinib better than immunocompromised mice. Other studies also suggested that lenvatinib has immunomodulatory capabilities, as treatment with this agent allowed immune cells to infiltrate the tumor better and activate NK cells.
Lenvatinib and sorafenib belong to the same drug category; however, the superior performance of lenvatinib in preclinical trials may be attributed to its ability to improve the immune antitumor response. Additional studies are needed to validate these findings using a large group of patients.
Changes in the neutrophil-lymphocyte ratio (NLR) and polymorphonuclear myeloid derived suppressor cells (PMN-MDSCs) have been reported in earlier research. These observations also necessitate additional research, as they were not measured in the current study.
While previous reports suggest that tumor cells express higher levels of chemokines and that NK cells exhibit an increased expression of adhesion molecules in mice treated with lenvatinib, the current study did not identify significant changes in cytokines associated with NK cell activity. Larger studies with more cytokine assays may elucidate this association.
NK cells are part of the innate immune response and destroy tumor cells by blocking their proliferation, growth, and migration. Considering the risk of immune evasion in some cancers, chimeric antigen receptor (CAR)-modified NK cells have been used to enable NK cells to perform their cytotoxic function in such tumors.
Considering the effect of lenvatinib on NK cells, sequence or combination therapies of lenvatinib with CAR-NK cell therapy are expected to show synergy in patients with thyroid cancer.”
- Jin, M., Kim, C. A., Bae, D. J., et al. (2023). Changes in peripheral blood immune cell population in thyroid cancer patients treated with lenvatinib. Scientific Reports. doi:10.1038/s41598-023-39503-w. https://www.nature.com/articles/s41598-023-39503-w
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News | Pharmaceutical News
Tags: Angiogenesis, Antigen, Assay, Blood, Cancer, Carcinoma, Cell, Cell Proliferation, Chemokines, Chimeric Antigen Receptor, Cytokine, Cytokines, Drugs, Efficacy, Fibroblast, Growth Factor, Hepatocellular Carcinoma, Immune Response, immunity, Immunomodulatory, Interleukin, Lymphocyte, Monocyte, Platelet, Preclinical, Proliferation, Receptor, Research, Sorafenib, Thyroid, Thyroid Cancer, Tumor, Tumor-Associated Macrophages, Vascular

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.