In a recent study posted to the medRxiv* pre-print server, Austrian researchers performed a multi-cohort analysis to investigate the slow resolution of subjective olfactory dysfunction (OD) and accompanying taste disorder in coronavirus disease 2019 (COVID-19) inpatients and outpatients.
 Image Credit: Microgen / Shutterstock
Image Credit: Microgen / Shutterstock
Background
The medical community has coarsely defined COVID-19-related persistent symptoms; however, these definitions do not characterize these symptoms. The characterization of COVID-19 recovery patterns, persistent symptoms, including OD and taste disorders, and their burden, are crucial to identifying at-risk patients who may benefit from targeted remedial therapies.
COVID-19-related OD occurs due to injured upper respiratory epithelial cells or neurons of the olfactory bulb, mucosa, or primary olfactory cortex and is estimated to affect up to 48% of patients during acute COVID-19. Note that the patients infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) wild type (wt), Alpha, and Delta variants more commonly suffer from OD.
There is data evidence that OD resolves within two to three weeks in most patients but may persist up to six months in five to 11% of patients; therefore, classified as post-acute sequelae of COVID-19 (PASC). Although this condition does not pose problems for all the patients, it affects the quality of life (QoL) due to its disabling character in some patients.
About the study
In the present study, researchers investigated the recovery trajectory, including clinical and psychosocial recovery of COVID-19 patients focusing primarily on OD. To this end, they re-analyzed the observations and results of a published survey of non-hospitalized COVID-19 patients and another multi-center study that had both ambulatory and hospitalized patients using association mining and clustering algorithms.
The ambulatory COVID-19 convalescents in Tyrol, Austria (AT), and South Tyrol, Italy (IT) participated in the Health after COVID-19 in Tyrol (HACT) online survey between 30 September 2020 and 5 July 2021. During this time, the SARS-CoV-2 Alpha variant dominated these regions along with the wt strain. Additionally, the team included patients with symptomatic COVID-19, with more than 90 days gap between diagnosis and survey completion in the analysis. They asked the participants to assign 42 symptoms to pre-defined duration classes as acute, long COVID, and PASC. They surveyed self-perceived complete recovery, need for rehabilitation, and drugs since COVID-19 as yes or no items.
The researchers used the partitioning around medoids (PAM) algorithm to cluster the training HACT AT cohort by symptom-specific recovery times and the five-nearest neighbor's classification algorithm to assign the IT cohort participants to the AT cohort-defined clusters.
The other study termed CovILD included both COVID-19 outpatients and inpatients recruited in Austria between March and June 2020. The team prospectively recorded eight symptoms, including reduced physical activity, hyposmia or anosmia, dyspnea, sleep problems, fever, cough, night sweating, and gastrointestinal symptoms on days 60-, 100-, 180- and 360 after COVID-19. They used the 16-item Sniffin' Sticks identification test to assess objective OD at the 100- and 360-day follow-up.
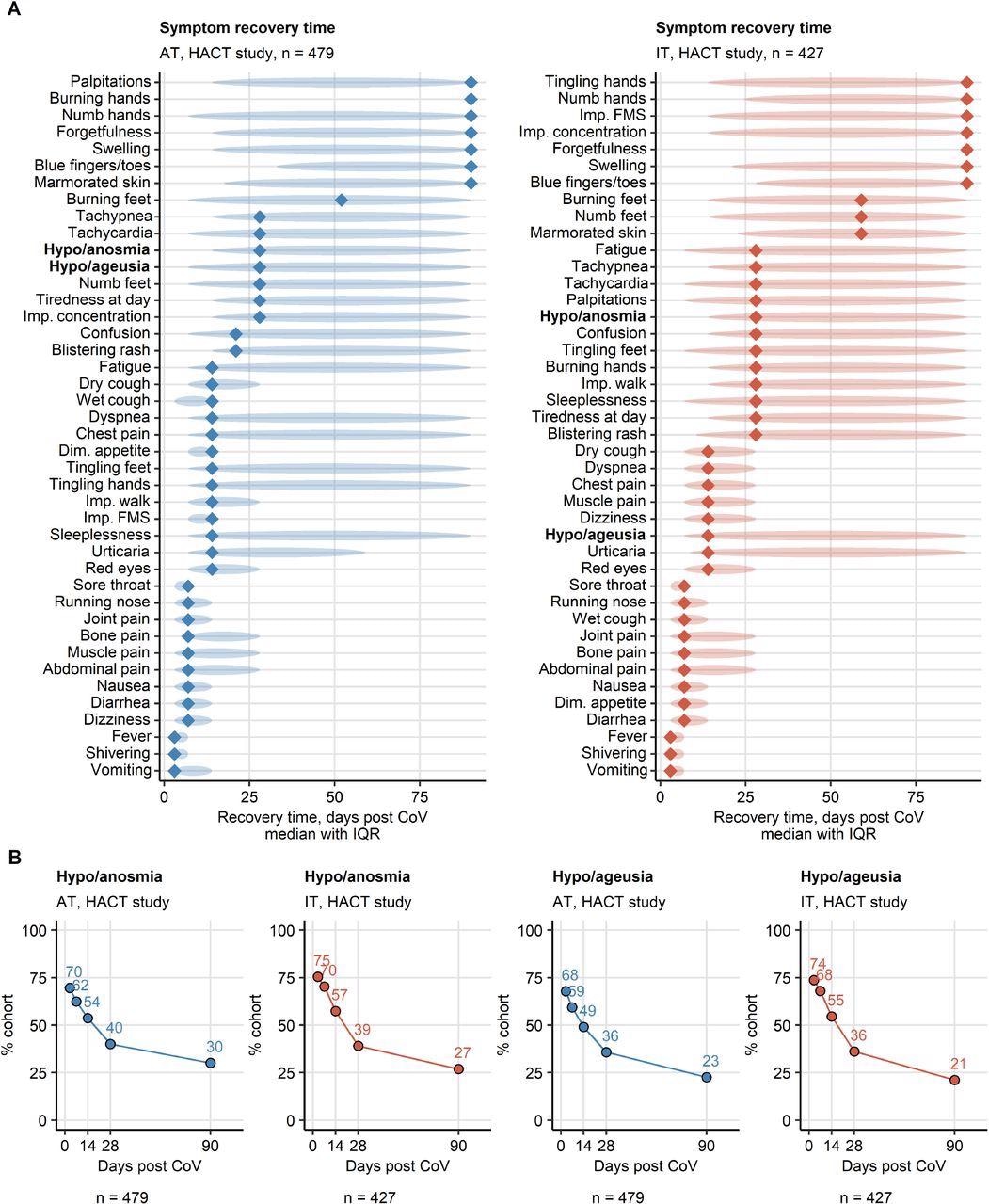
Symptom-specific recovery times in ambulatory COVID-19. Symptom-specific recovery times were calculated for each participants of the HACT study cohorts (Austria: AT, Italy: IT). Imp.: impaired, Dim.: diminished, FMS: fine motor skills. (A) Distribution of the recovery times in the individuals with the indicated symptoms present during acute COVID-19. Diamonds represent median recovery times, tinted ellipses code for interquartile ranges. Numbers of complete observations are indicated in the plot captions. (B) Percentages of individuals with smell and taste disorders in the AT (Austria) and IT (Italy) HACT study cohorts at particular time points after clinical onset. Numbers of complete observations are indicated under the plots.
Study findings
Self-perceived OD was a common acute symptom among 47 to 75% of ambulatory patients and 33 to 53% of patients suffering from moderate-to-severe COVID-19. Interestingly, taste disorders accompanied its slow-pace recovery in these patients.
Convalescents with persistent OD were predominantly young females with only a few pre-existing chronic conditions; who enjoyed good mental and physical health. Consequently, female patients with OD may best benefit from early neurological assessment for timely initiation of therapy. Moreover, the first four weeks of being convalescent halved the percentages of self-perceived OD; however, every sixth moderately ill COVID-19 patient of the CovILD cohort reported persistent OD at the one-year study follow-up.
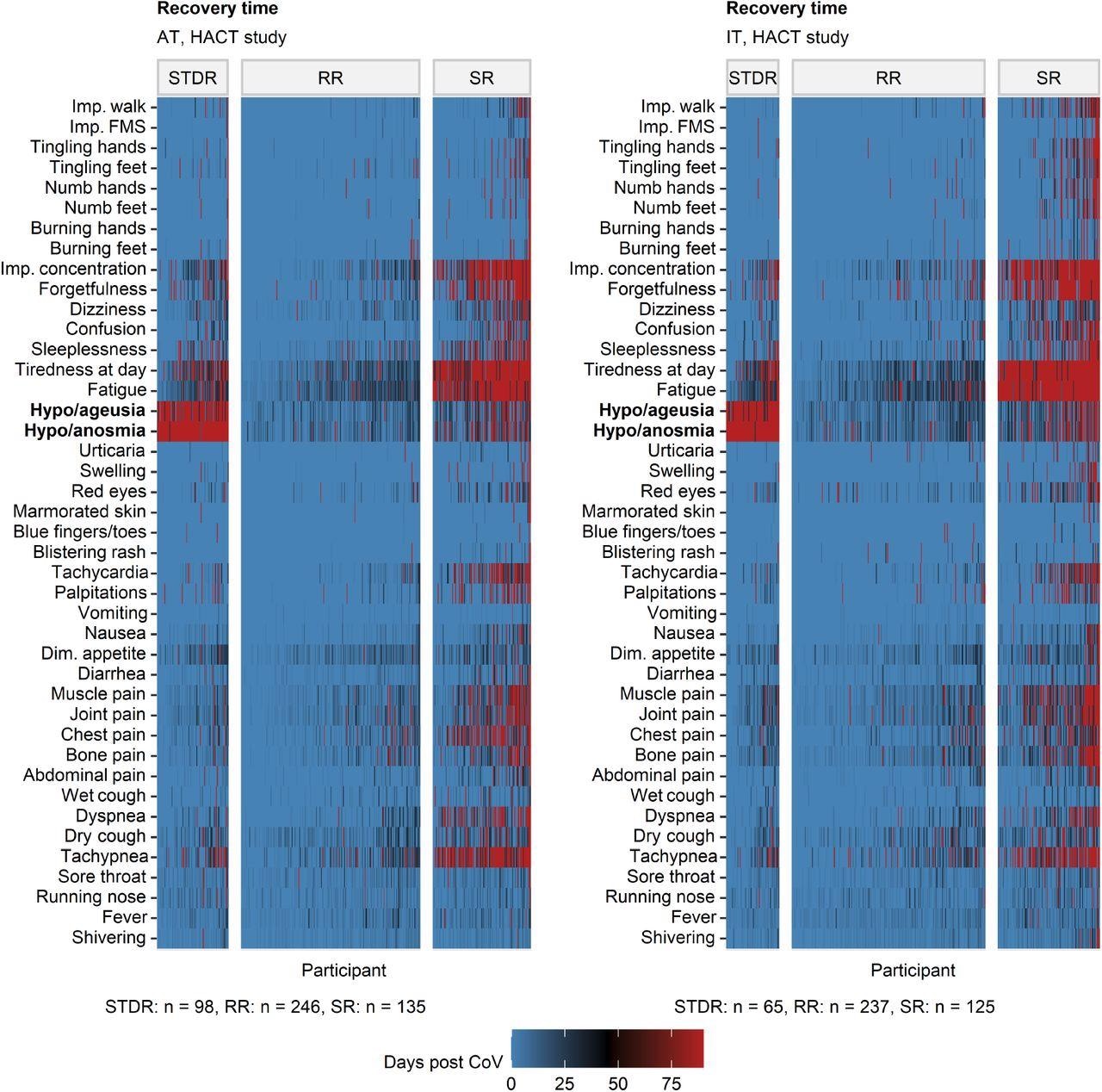
Clustering of ambulatory COVID-19 individuals by symptom-specific recovery times. Individuals of the training Austria (AT) cohort of the HACT study were subjected to clustering in respect to symptom-specific recovery times with the PAM (partitioning around medoids) algorithm and Euclidean distance measure (Supplementary Figure S8). Cluster assignment in the test Italy (IT) HACT cohort was done with k-NN label propagation algorithm. Recovery times for particular COVID-19 symptoms in the COVID-19 recovery clusters are presented as heat maps. Numbers of individuals assigned to the recovery clusters are indicated under the plots. Dim.: diminished, Imp.: impaired, FMS: fine motor skills.
The researchers used questionnaires specifically addressing OD-related QoL measures. Adopting a different methodology might have resulted in discrepant results. Accordingly, persistent OD affected a subset of patients with no other clinical, physical, or mental health issues.
The study showed a unique OD recovery kinetics with fast resolution within the first few weeks, followed by a plateau. Therefore, it is unknown whether post-COVID-19 OD resolves in all patients. Since complete OD resolution might require months to years, it might have left millions of COVID-19 convalescents worldwide with residual OD. Hence, there is an immediate need to develop novel therapeutics to treat this condition. Studies have demonstrated that olfactory training may significantly amend OD in patients with COVID-19 and traumatic brain injury (TBI). Interestingly, COVID-19-independent objective OD prevalence is as high as 29% in the general population. Therefore, presumably, the CovILD cohort had a higher objective OD rate than self-perceived hyposmia. Further research is needed to elucidate the observed underestimates of the objective OD frequency during long-term COVID-19 recovery.
Conclusions
The study identified OD, taste disorders, tiredness, fatigue, and neurocognitive symptoms as the top clinical manifestations of long COVID and PASC. Of these symptoms, persistent smell and taste disorders, which also reflected an impaired retronasal smell, qualified as a distinct phenotype of long COVID and PASC. However, the overlap of OD and taste disorders with other persistent symptoms was lesser, especially 90 days after COVID-19 onset.
To conclude, the observed OD phenotype characterized by the absence of physical or mental health deficits stressed the heterogeneity of PASC. Nevertheless, there is a continuous need for phenotyping of COVID-19-related OD as new SARS-CoV-2 variants continue to emerge.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Distinct smell and taste disorder phenotype of post-acute COVID-19 sequelae, Verena Rass, Piotr Tymoszuk, Sabina Sahanic, Beatrice Heim, Dietmar Ausserhofer, Anna Lindner, Mario Kofler, Philipp Mahlknecht, Anna Boehm, Katharina Hüfner, Alex Pizzini, Thomas Sonnweber, Katharina Kurz, Bernhard Pfeifer, Stefan Kiechl, Marina Peball, Philipp Kindl, Lauma Putnina, Elena Fava, Atbin Djamshidian, Andreas Huber, Christian J Wiedermann, Barbara Sperner-Unterweger, Ewald Wöll, Ronny Beer, Alois Josef Schiefecker, Rosa Bellmann-Weiler, Herbert Bachler, Ivan Tancevski, Bettina Pfausler, Giuliano Piccoliori, Klaus Seppi, Günter Weiss, Judith Löffler-Ragg, Raimund Helbok, medRxiv pre-print 2022, DOI: https://doi.org/10.1101/2022.06.02.22275932, https://www.medrxiv.org/content/10.1101/2022.06.02.22275932v1
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Anosmia, Brain, Chronic, Coronavirus, Coronavirus Disease COVID-19, Cortex, Cough, Drugs, Dyspnea, Fatigue, Fever, Frequency, heat, Mental Health, Neurons, Phenotype, Physical Activity, Propagation, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sleep, Syndrome, Therapeutics, Tiredness, Traumatic Brain Injury

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article