In a recent article posted to the bioRxiv* preprint server, researchers at Rutgers, the State University of New Jersey, the University of South Florida, and the Catholic University of America demonstrated that the natural severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) main protease (Mpro) mutations result in nirmatrelvir resistance.
 Study: Naturally occurring mutations of SARS-CoV-2 main protease confer drug resistance to nirmatrelvir. Image Credit: Orpheus FX / Shutterstock
Study: Naturally occurring mutations of SARS-CoV-2 main protease confer drug resistance to nirmatrelvir. Image Credit: Orpheus FX / Shutterstock
Background
The ongoing SARS-CoV-2 pandemic emphasizes the urgency for orally bioavailable antiviral medications. The Mpro of the SARS-CoV-2 is a cysteine protease and a recognized target for antiviral drugs. Paxlovid (nirmatrelvir) and molnupiravir are the only two oral SARS-CoV-2 medications that have received Food and Drug Administration (FDA) approval. Paxlovid comprises the Mpro inhibitor nirmatrelvir and the metabolic enhancer ritonavir.
The risk of hospitalization or death was 89% lower in coronavirus disease 2019 (COVID-19) patients who received Paxlovid less than three days of the commencement of SARS-CoV-2 symptoms than in those who got the placebo. Nevertheless, the appearance of SARS-CoV-2 variants with Mpro mutations prompted concerns about probable drug resistance.
About the study
The present work sought to discover Mpro drug-resistant SARS-CoV-2 mutants associated with naturally occurring polymorphisms. The researchers examined the SARS-CoV-2 sequences in the Global Initiative on Sharing Avian influenza Data (GISAID) database.
The team examined the drug resistance of three Mpro inhibitors: PF00835231, GC-376, and nirmatrelvir. GC-376 was used for treating feline infectious peritonitis virus (FIPV) infection among cats. Further, Pfizer developed phosphonate PF-00835231 prodrug as an intravenous agent for treating COVID-19 patients in hospitals and was progressed to clinical trial. Finally, nirmatrelvir was the active ingredient in Paxlovid.
The authors concentrated on 12 Mpro active site residues, M49, H41, N142, T135, S144, H164, H163, M165, H172, E166, and Q189, found within 6 Å of the nirmatrelvir binding domain, i.e., PDB: 7SI9, to find drug-resistant Mpro mutants. They proposed that mutations across the active site residues directly impact substrate adherence and drug resistance. To test this theory, the researchers evaluated the mutations in these 12 residues utilizing the SARS-CoV-2 sequences from the GISAID.
The thermal shift binding assessment and an enzymatic assay based on fluorescence resonance energy transfer (FRET) were used to determine the drug sensitivity. The SARS-CoV-2 Mpro mutant proteins were expressed and examined for nirmatrelvir inhibition and enzymatic activity utilizing X-ray crystal structures.
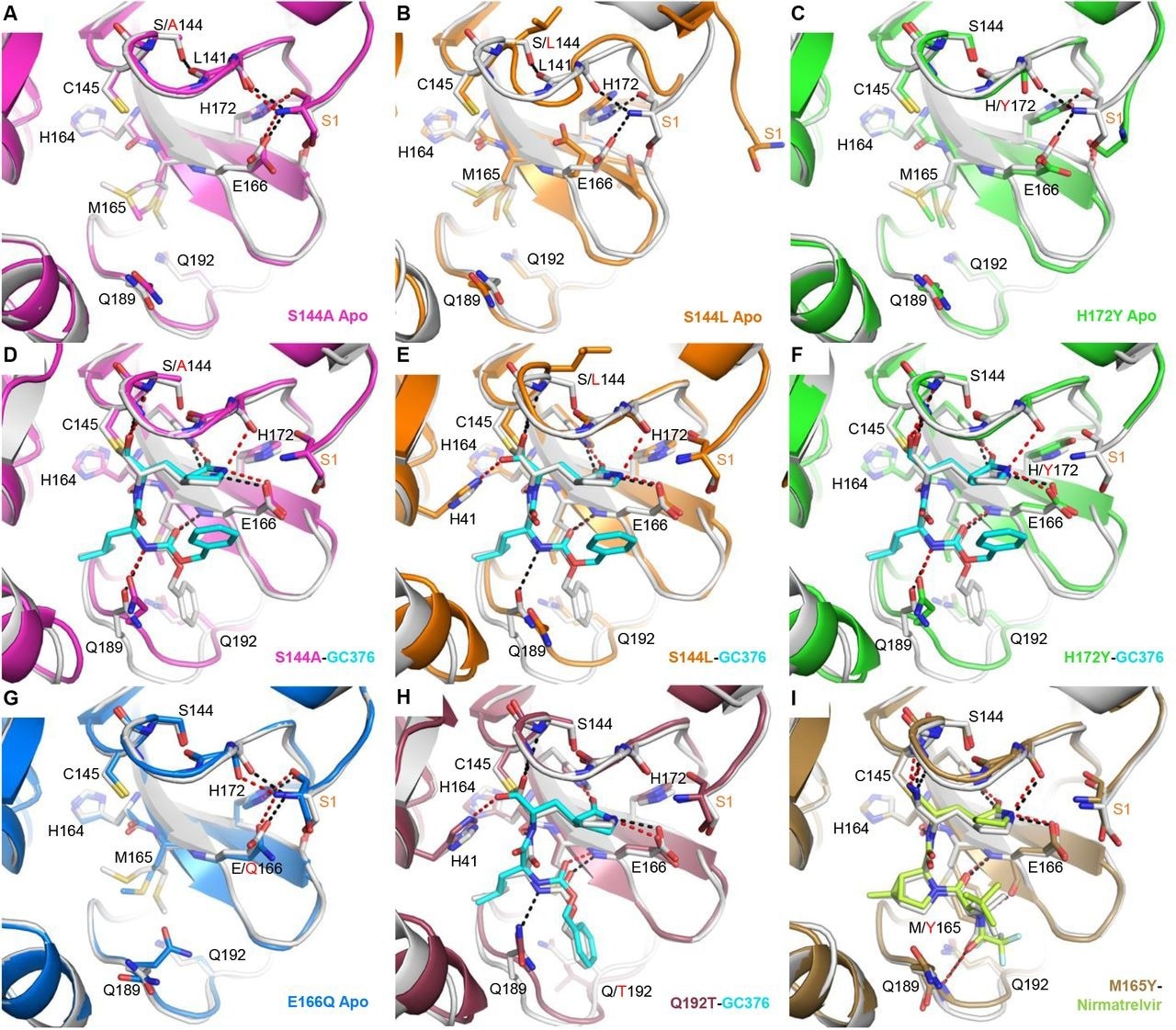
X-ray crystal structures of Mpro mutants. Each mutant structure is aligned with the corresponding WT structure shown in white (apo, PDB 7JP1; GC-376 complex, 6WTT; nirmatrelvir complex, 7RFW). For the mutant structures, GC-376 and nirmatrelvir are shown in cyan and neon green respectively. WT HBs are shown as black dashes for selected residues at the mutation sites or between the protein and inhibitor. Mutant HBs are shown as red dashes. Mutations are indicated with red text. S1 residue from the N-terminus of the adjacent protomer is labeled in orange. The side chain of L141 is not shown. (A) Apo Mpro S144A (magenta, PDB 8D4L). (B) Apo Mpro S144L (orange, PDB 8DFE). The view for panel B is shifted slightly to show for the movement of the adjacent N-terminus. (C) Apo Mpro H172Y (green, PDB 8D4J). (D) Mpro S144A GC-376 complex (magenta, PDB 8D4M). (E) Mpro S144L GC-376 complex (orange, PDB 8DD9). (F) Mpro H172Y GC-376 complex (green, PDB 8D4K). S1 residue is disordered. (G) Apo Mpro E166Q (blue, PDB 8D4N). (H) Mpro Q192T GC376 complex (mauve, PDB 8DGB). (I) Mpro M165Y Nirmatrelvir complex (brown, PDB 8DCZ).
Results
The authors found 66 common SARS-CoV-2 Mpro mutations positioned at the nirmatrelvir binding site, spanning all high-frequency mutants at the 12 analyzed residues.
According to the kcat/Km value for enzymatic activity and the Ki value for drug resistance, the Mpro mutants were divided into three categories: category 1 contains essential residues for enzymatic activity (H163 and H41); category 2 contains hot spot residues for drug resistance (M165, S144, H172, E166, and Q192); and category 3 comprises residues that can withstand multiple mutations without substantially influencing drug inhibition and the enzymatic activity (M49, T135, N142, Q189, and H164).
Most Mpro mutants exhibited diminished enzymatic activity, i.e., kcat/Km greater than a 10-fold decrease. On the other hand, 11 mutants, including M165T, S144M/F/A/G/Y, H172Q/F, E166Q, and Q192T/S/V, displayed similar enzymatic activity as the SARS-CoV-2 wild-type strain with kcat/Km less than a 10-fold modification and resistance to nirmatrelvir with Ki greater than a 10-fold hike.
Although the enzymatic activity of several single mutants found in this investigation was decreased, it was conceivable that the virus could produce multiple mutations, such as the H172Y/Q189T mutant, assisting in the restoration of replication fitness, maintain or even improve drug resistance.
Besides, the X-ray structures illustrated how Mpro mutations influenced the conformational stability of the active site, lowering ligand binding. X-ray structures of six single mutants with or without nirmatrelvir/GC-376 were established.
The team noted that the mutants take on a productive configuration when a substrate or inhibitor is present, which explains how they can catalyze the reaction. The reduction in the catalytic properties of the mutants and inhibition by nirmatrelvir/GC-376 appears to be caused by two factors: an entropic effect due to the active site's increased conformational instability and an enthalpic impact caused by the direct disruption of ligand-binding contacts.
Conclusions
Overall, in the current research, the authors found 66 drug-resistant Mpro mutants arising from natural SARS-CoV-2 polymorphism from the GISAID database. These mutations may impact the effectiveness of Paxlovid, and continuous Paxlovid prescription might probably elevate the prevalence of these pre-existent drug resistance mutants.
The nirmatrelvir resistance hotspots, Mpro M165, S144, H172, E166, and Q192 mutants, need to be monitored actively across the circulating SARS-CoV-2s. Most likely, mutations at these residues will result in considerable drug resistance while maintaining the enzyme function. Whether these mutations reduce the viral replication capacity and transmission needs further assessment.
Double or triple mutants may arise to counteract the loss of enzymatic function from the single mutant while improving or maintaining drug resistance, as seen by the H172Y/Q189T mutant. As a result, it is vital to track the Mpro mutants with decreased enzymatic activity from the current study.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Naturally occurring mutations of SARS-CoV-2 main protease confer drug resistance to nirmatrelvir; Yanmei Hu, Eric M Lewandowski, Haozhou Tan, Ryan T Morgan, Xiujun Zhang, Lian M Jacobs, Shane G Butler, Maura V Mongora, John S Choy, Yu Chen, Jun Wang. bioRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.06.28.497978, https://www.biorxiv.org/content/10.1101/2022.06.28.497978v1
Posted in: Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Assay, Avian Influenza, Clinical Trial, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cysteine, Drugs, Enzyme, Fluorescence, Food, Frequency, FRET, Influenza, Ligand, Mutation, Pandemic, Peritonitis, Placebo, Protein, Research, Respiratory, Ritonavir, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus, X-Ray

Written by
Shanet Susan Alex
Shanet Susan Alex, a medical writer, based in Kerala, India, is a Doctor of Pharmacy graduate from Kerala University of Health Sciences. Her academic background is in clinical pharmacy and research, and she is passionate about medical writing. Shanet has published papers in the International Journal of Medical Science and Current Research (IJMSCR), the International Journal of Pharmacy (IJP), and the International Journal of Medical Science and Applied Research (IJMSAR). Apart from work, she enjoys listening to music and watching movies.
Source: Read Full Article