A pioneering lung cancer study, led by the University of Birmingham’s Cancer Research UK Clinical Trials Unit, has highlighted important factors that will need to be considered in the next wave of precision medicine studies particularly in treating genomically complicated cancers.
Published in Nature, the National Lung Matrix Trial (NLMT) is the world’s largest precision medicine clinical trial for non-small-cell lung cancer (NSCLC) patients, funded by Cancer Research UK (CRUK) and supported by the charity’s Stratified Medicine Program Phase 2 (SMP2) screening platform.
A £25 million collaboration with Pfizer, AstraZeneca and other pharmaceutical companies, and with support from the NHS, the NLMT matches different treatments to different groups of patients based on genetic changes in their cancer.
Using an innovative trial design that incorporates multiple treatment arms, NLMT allows for a more flexible and informed approach than traditional clinical trials. Each arm tests a different targeted treatment matched to a different genetic subtype of NSCLC.
The trial’s adaptive approach makes it possible for new drugs and combinations to be added as soon as they become available or retired quickly and easily if evidence suggests they aren’t effective.
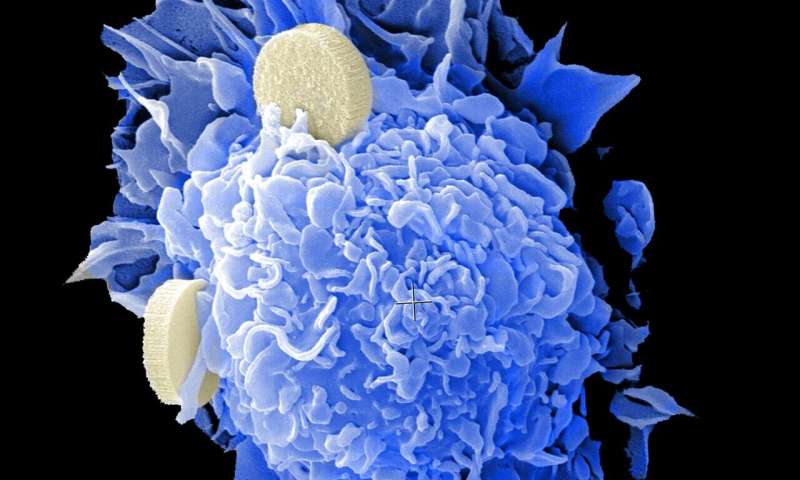
Patients who sign up to take part in NLMT are genetically screened by the Cancer Research UK SMP2 to understand more about their tumor type, and whether they possess the relevant genetic signatures to be matched to a targeted treatment.
Since the trial opened to recruitment in May 2015 until November 2019, 288 patients have been recruited to the 19 targeted treatment cohorts on the trial.
Results revealed key learnings on the use of precision medicine, such as how the appropriate pre-clinical work is essential in defining appropriate biomarker-drug combinations to test in the clinic, on ensuring that the best drugs available are used to hit the genomic targets, the scale of attrition from large screening platforms, and the importance of analyzing and publishing outcome data of an ongoing study.
The attrition rate was high with only a 5% of SMP2 patients receiving treatment on NLMT. As trials often come towards the end of the patient journey, cancer progression might make patients too unwell to be recruited onto trials. Targeted therapy trials should take place much earlier in the cancer journey and use blood based genomic testing for fast turn-round of the information needed to match patients to drugs.
Lead author Professor Gary Middleton, Medical Oncologist at the University of Birmingham said: “This study provides data on how the next wave of trialing targeted therapies to treat complex cancers should be designed. This is the first trial of its kind, the novel Bayesian design allows outcome data from open cohorts that are still recruiting to be reported alongside closed cohorts, whereas previous umbrella studies have only published the results of completed arms and cohorts.
“We found genomically complicated tumors are hard to treat with targeted therapy, especially with monotherapy. The models we test drugs on are too simplistic—they don’t represent the genomic complexity of the tumor, or the trajectory of how they rapidly evolve. We need models that take into account the complexity and trajectory of a human tumor to decide if a drug is going to work.”
Professor Pam Kearns, Director of Birmingham’s CRUK Clinical Trials Unit and University of Birmingham’s Institute of Cancer and Genomic Sciences, said “The National Lung Matrix Trial is a landmark complex innovative design trial and represents a step-change in our understanding of how to develop precision medicine in challenging to treat cancers.”
Dr. Ian Walker, Director of Research at Cancer Research UK said: “The National Lung Matrix trial is a flagship program for Cancer Research UK and continues to provide significant insights into how we should treat genomically diverse cancers, such as lung. Not only will it shape the thinking for future studies delivering complex precision medicines, but it has also demonstrated how molecular diagnostic testing and clinical research can work in a truly integrated manner within the National Health Service across the UK to allow patients to access the latest new treatments.”
NLMT patient Paul Inett, 72 years old, said “I was diagnosed with stage four metastatic lung cancer in late April 2015 that had spread to glands in my chest. I was referred to Professor Gary Middleton at the Queen Elizabeth Hospital Birmingham and was recruited onto the National Lung Matrix Trial. Fortunately my biopsy showed a genetic marker that matched to one of the treatment arms on the trial and received a targeted cancer drug. This ground breaking research saved my life. I’m now able to live a relatively active life including spending time with my family and taking exercise classes at my local gym”.
Source: Read Full Article