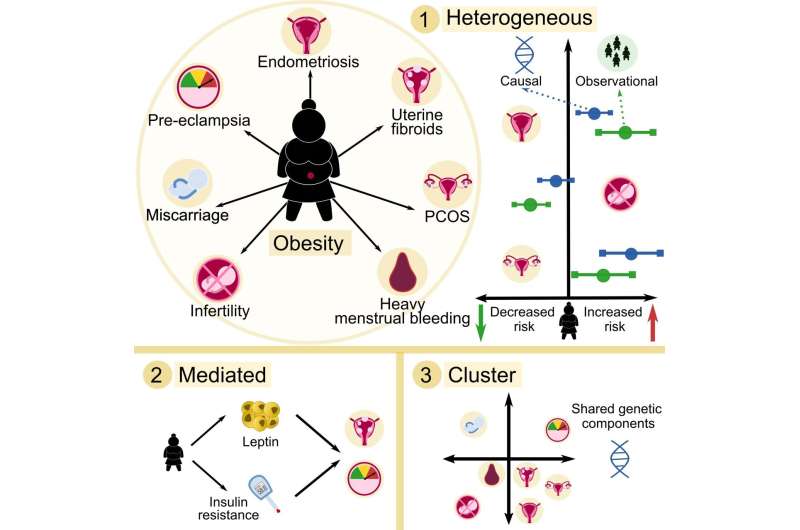
Obesity is associated with an increased risk of developing female reproductive disorders, however, the roles and mechanisms of obesity in the cause(s) of reproductive conditions are unclear. A study publishing February 1st in PLOS Medicine by Samvida Venkatesh at University of Oxford, United Kingdom and colleagues suggests an etiological link between obesity and a range of female reproductive conditions, but the extent of this link differs among conditions.
Female reproductive disorders are common conditions affecting the health and well-being of many. However, the role of obesity in the development of female reproductive conditions is under-studied. To investigate the causal associations between obesity, metabolic hormones, and female reproductive disorders, researchers conducted a Mendelian randomization study of 257,193 women of European ancestry aged 40-69. They accessed records from UK Biobank, a large-scale biomedical database containing the medical, environmental, and genetic information of participants. The researchers then created a statistical model to estimate the association of body mass index and waist-to-hip ratio with risk of numerous female reproductive conditions including endometriosis, heavy menstrual bleeding, pre-eclampsia, and infertility.
The researchers found observational associations between obesity and a range of female reproductive disorders, including uterine fibroids, polycystic ovary syndrome, heavy menstrual bleeding, and pre-eclampsia. They also found that some inherited genetic variation associated with obesity is also associated with female reproductive disorders, but the strength of those associations differed by type of obesity and reproductive condition. The study had several limitations, such as the low prevalence of female reproductive disorders among participants, and a lack of body mass index and waist-hip-ratio data prior to disease onset.
Source: Read Full Article