A new targeted treatment has been recommended by the National Institute of Health and Care Excellence (NICE) for some adults with advanced high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer
Niraparib will be available through the Cancer Drugs Fund as a maintenance treatment to enhance or prolong the effect of initial treatment. In this case, niraparib will be used after platinum-based chemotherapy for people with and without BRCA mutations.
How does niraparib work?
Niraparib is a type of targeted cancer drug known as a PARP inhibitor.
Cancer Research UK researchers were involved in some of the earliest work into PARP inhibitors, which aim to kill cancer cells by stopping them repairing damaged DNA, in the early 1990’s.
PARP is a protein found in our cells that helps damaged cells to repair themselves. Cancer cells rely on PARP proteins to keep their DNA healthy to keep on growing and dividing.
As a cancer treatment, these inhibitors stop PARP from doing its repair work in cancer cells and the cell dies. PARP inhibitors were first trialed in combination with drugs that caused DNA damage—such as chemotherapy—to heighten the effects of these treatments.
But researchers quickly realized the potential of these drugs to treat cancers that already had problems repairing cell damage, focusing on cancers with a change in genes known as BRCA.
Normally, BRCA1 and BRCA2 instruct cells to make proteins that help repair damaged DNA. Cells are less likely to repair themselves properly if they have a fault in one or both of these genes and people who have faulty BRCA genes have an increased risk of prostate, breast and ovarian cancer.
Cancer cells with BRCA gene faults already have a poor repair system. So blocking PARP with a PARP inhibitor drug in these cells causes DNA damage to accumulate, pushing cells over the edge.
What the clinical trials tell us
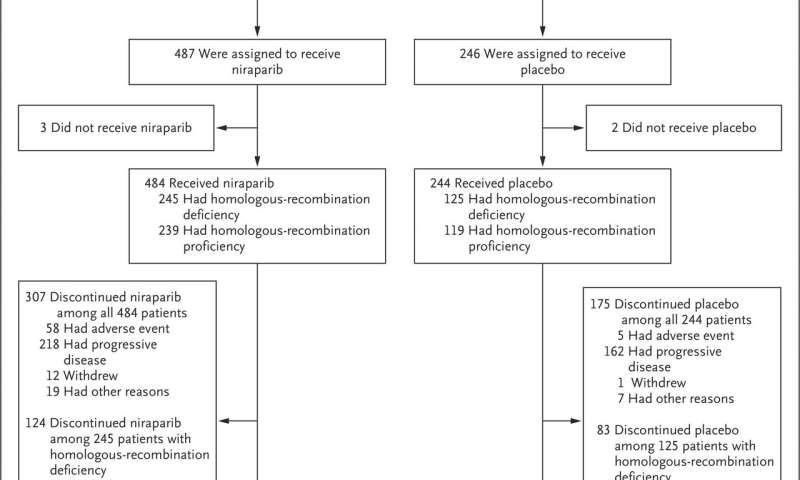
Evidence from a large clinical trial shows that niraparib can give people who have already responded well to an initial round of platinum-based chemotherapy more time before their cancer gets significantly bigger.
During the clinical trial, people taking niraparib lived for an average of 13.8 months without their cancer getting bigger, compared to 8.2 months with a placebo.
Further analysis also indicated that niraparib increases the average amount of time before somebody’s cancer gets bigger for people whose cancer doesn’t have an error in either BRCA1 or BRCA2 genes, where there are currently no maintenance treatments available after initial treatment.
The PRIMA trial hasn’t been running for long enough to determine if niraparib can extend survival for people with high grade epithelial ovarian, fallopian tube or primary peritoneal cancers. The trial is still ongoing and further data could help to reduce uncertainties about the long-term impact of niraparib.
Clinical experts who helped make the decision explained that there is a high unmet need for more maintenance treatment options after first-line treatment for advanced cases of ovarian cancer.
“Evidence from clinical trials suggests that niraparib can delay the progression of someone’s cancer, potentially delaying the need for more chemotherapy and improving their quality of life. Because niraparib has been approved for use through the Cancer Drugs Fund, people will have access whilst more evidence on its longer-term benefits is gathered,” says Shrotri.
Long-term benefits
Uncertainties around the long-term benefits of treatment with niraparib meant it could not be recommended for routine use in the NHS at this time. However, its potential to be a cost-effective use of NHS resources meant niraparib could be approved via the Cancer Drugs Fund.
The Cancer Drugs Fund is a way for NHS England to give people access to new medicines while more data is collected on their long-term benefits.
Source: Read Full Article