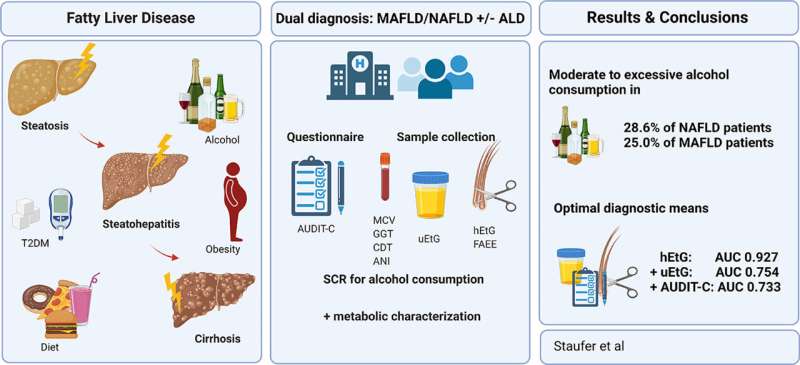
It is important to know whether patients have non-alcoholic fatty liver disease (NAFLD) or alcohol-related liver disease (ALD), as this distinction plays a key role in treatment and prognosis but cannot be reliably determined by established diagnostic means. In a study led by MedUni Vienna, a new method has now been used to determine alcohol consumption in fatty liver disease. It was found that about 30% of patients with presumed NAFLD were at risk of alcohol-related liver damage. Alcohol markers in the patients’ hair proved to be particularly accurate indicators. The research was recently published in the Journal of Hepatology.
The study assessed the alcohol consumption of 184 patients being treated for NAFLD or ALD in the specialized hepatology outpatient clinics of University Hospital Vienna and other centers in Oberndorf and Vienna. The research team led by Katharina Staufer and Michael Trauner, Head of the Division of Gastroenterology and Hepatology at MedUni Vienna and University Hospital Vienna, compared the results from currently available methods of alcohol detection with the results from a new testing procedure. This involves combining the alcohol parameters ethyl glucuronide in hair (hEtG) and urine (uEtG) with the AUDIT-C (Alcohol Use Disorders Identification Test) questionnaire. Using this method, repeated moderate to excessive alcohol consumption was detected in about 29% of patients with alcohol-related liver disease but also in about 29% of patients with presumed non-alcoholic fatty liver.
25% of the population is diagnosed with NAFLD
Non-alcoholic fatty liver disease is associated with obesity and insulin resistance as part of metabolic syndrome and is identified in up to 25% of the population. This makes NAFLD the most commonly diagnosed chronic liver disease in the world today. A diagnosis of NAFLD requires the exclusion of harmful amounts of alcohol as a cause.
Medical research has not yet fully established what influence low to moderate alcohol consumption has on the development and progression of fatty liver disease. On the other hand, patients with an alcohol consumption of > 60 g ethanol/day (equivalent to approximately 1.5 liters of beer or 0.75 liters of wine/day) have been shown to develop serious sequelae such as steatohepatitis (fatty liver hepatitis), fibrosis (liver scarring), and even cirrhosis. Recent studies assume significantly lower potentially harmful alcohol levels of 10–20 g ethanol/day, above which alcohol-related liver disease cannot be reliably ruled out.
Removing the social stigma is important to identify potentially harmful alcohol consumption in fatty liver patients at an early stage, so that the optimal treatment can be recommended. However, this is often problematic in clinical practice, since patients often fail to report or underreport their consumption of alcohol—either because they retrospectively underestimate how much they drink, are afraid of being stigmatized or as part of an alcohol use disorder.
“Measuring ethyl glucuronide in hair and urine in addition to using the AUDIT-C questionnaire can help to determine alcohol consumption and thus, for the first time, enable a frank conversation about actual alcohol consumption and its consequential damage,” explains lead author Katharina Staufer (Division of Transplantation at MedUni Vienna/University Hospital Vienna), stressing the importance of a trusting doctor-patient relationship. “We need to remove the social stigma that still often accompanies alcohol-related liver damage and provide the best possible treatment.”
Source: Read Full Article