In the condition known as cavernoma, lesions arise in a cluster of blood vessels in the brain, spinal cord or retina. Researchers at Uppsala University show in a new study that white blood cells and protein structures associated with the immune response infiltrate the vessel lesions. The findings support that inflammation has a role in the development of cavernoma and indicate a potential biomarker for the disease.
The vascular lesions, or blood-vessel malformations, that appear in a cerebral cavernoma—also known as a cerebral cavernous malformation (CCM) resemble mulberries. They bleed easily, which may cause epileptic attack, neurological problems and stroke. The condition is due to genetic mutations that may be inherited or occur spontaneously, and is incurable at present.
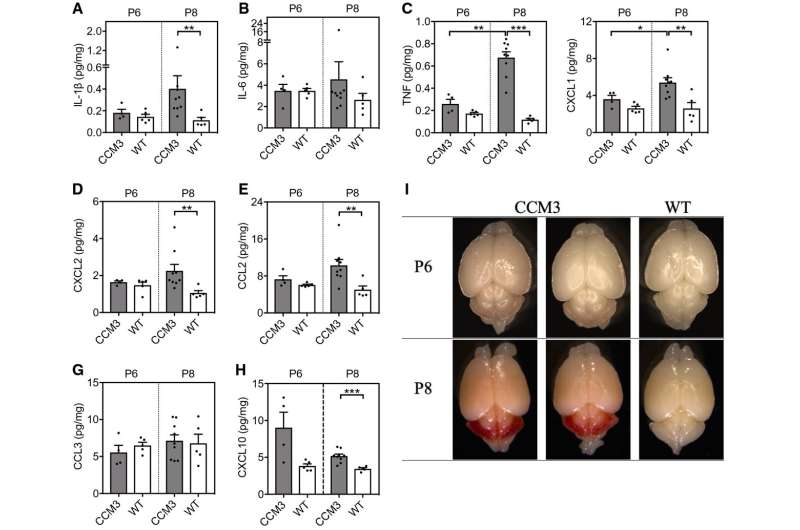
Research in recent years has suggested that inflammation is involved in CCM. I the new study, the researchers have examined in detail which immune cells respond in CCM. They could also show for the first time that net-like protein structures called NETs are formed in CCM. NETs (Neutrophil Extracellular Traps) are made up of cell nuclei and cell structures and are associated with the immune response.
“We have used genetically modified mice where a mutated form of a certain gene results in CCM. We found that neutrophils, a type white blood cell, are the first to be recruited to the vessel lesions in mice with CCM. In addition, we detected NETs both in the brain and circulating in the blood. In mice without CCM we didn’t find any NETs,” says Peetra Magnusson, Associate Professor at the Department of Immunology, Genetics and Pathology at Uppsala University, who has led the study.
NETs normally act as a defense in the body by capturing and destroying intruders such as bacteria. High levels of NETs have previously been shown in cancer patients and they are an important component in COVID. These net-like structures can cause vessel damage and the formation of blood clots. Their role in CCM has not been clarified but when the researchers tested a treatment that degraded the NETs, the CCM-related vessel damages were reduced.
The researchers could also detect NETs in brain tissues from patients with CCM, both the inherited form and the one that occurs spontaneously.
Source: Read Full Article