Huntsman Cancer Institute researchers discovered people with a certain polyp syndrome and their first-degree relatives are at increased risk for colorectal cancer. In addition, people with certain colon lesions are also at an at increased risk. Lead authors Karen Curtin, Ph.D., epidemiologist at Huntsman Cancer Institute and associate professor of internal medicine at the University of Utah (U of U), and Priyanka Kanth, MD, associate professor of internal medicine at MedStar Georgetown University Hospital and adjunct associate professor of internal medicine at the University of Utah, answer questions about the study published in The American Journal of Gastroenterology.
What are serrated polyposis syndrome (SPS) and sessile serrated lesions (SSL)? How do they increase the risk of colorectal cancer?
SPS is a condition where patients have multiple jagged-edge polyps. Less than 1% of patients who get a colonoscopy have this condition. The risk of colorectal cancer is 25–40% higher in patients with SPS. Studies suggest SPS is inherited, although the source is unknown.
An SSL is a type of abnormal, jagged-edge tissue or growth found in 3–8% of people screened for colorectal cancer. These lesions are larger and less common than conventional polyps. SSLs carry a greater risk of colorectal cancer, as they are more difficult to detect.
What was the goal of this study?
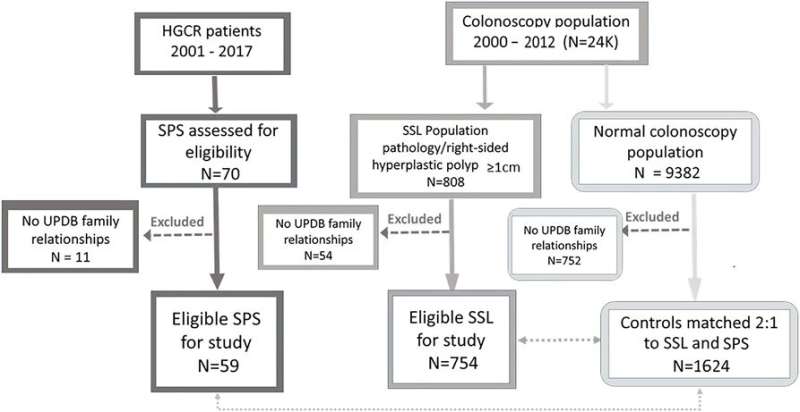
To study the risk of colorectal and other common cancers in patients with SPS and SSL and their families. This was possible because of the Utah Population Database. This unique resource provides information on multiple generations of families and their colonoscopy records. Patient privacy is protected and individuals cannot be identified.
What prompted the idea for the study?
Our shared interests in studying the risk of colorectal and other cancers in SPS and SSL patients.
There are no population-wide studies that have looked at the risk of colorectal and other common cancers in the relatives of SSL patients and very few studies have examined relatives of SPS patients. Given the availability of the Utah Population Database, we had an advantage to study this topic that can impact families.
What is the significance of your findings?
We confirmed a high risk of colorectal cancer in patients and close relatives (parents, siblings, children) with SPS and found no evidence of risk in more distant relatives (grandparents and cousins). We also found no evidence of increased risk of breast, pancreas, and prostate cancer in people with SPS or their close relatives.
Our most significant finding was that all family members of individuals with SSL may also have an increased risk of colorectal cancer if the SSL patient also had a non-cancerous adenoma or precancerous cells were found during an exam. Relatives of patients with an advanced non-cancerous tumor are recommended to undergo early colonoscopy screening at age 40. Our findings also suggest relatives of patients with SSL should undergo screening before age 50.
How might this information lead to improvements in prevention or treatment?
SPS patients and their close relatives should begin colonoscopy screenings earlier, and have them more frequently, than currently recommended. Relatives of patients with SSL with any pre-cancerous adenoma should also consider early screening. There are no current guidelines and we hope our findings can help formulate them.
What are the next steps for this research?
Source: Read Full Article