As COVID-19 looks more like a disease of the immune system, a Michigan engineer is working with doctors to look at how immune responses differ between mild and severe cases.
A chemical engineer who studies the immune system has set to work on COVID-19, working on a vaccine but also collaborating with doctors to understand the details of immune responses at the cellular level.
“What makes some groups more susceptible than others? If we can understand that, that could really help us design better vaccines and treatments,” said Fei Wen, the associate professor of chemical engineering who is undertaking the projects.
COVID-19 has been described in The Atlantic as a disease of the immune system, owing to the way that the most serious symptoms are related to an overactive immune response rather than the virus itself. Therefore, to understand and rein in the immune response, it would be useful to know exactly what’s going on.
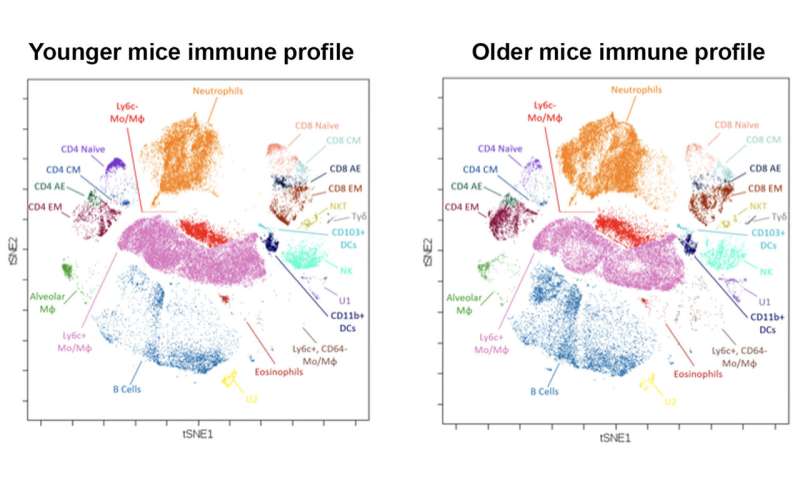
Wen’s lab has a machine that can extract that kind of information from blood. Her team uses metal particles to tag a hundred or so different biomarkers—typically proteins—on an individual cell. Then, they run each cell through a machine that tears it apart and uses the metals to sort out how much of each protein was present.
This method reveals not only which immune cells are present but also their numbers and their functional state. Just because an immune cell is there doesn’t mean it’s in fighting form. These snapshots of the immune system could be used to compare what is happening inside a person who has a mild form of COVID-19 to someone who has been hospitalized. It can compare the response of someone who survives to that of someone who does not.
The medical lead on the project is Daniel Goldstein, M.D., the Eliza Maria Mosher Collegiate Professor in Internal Medicine.
“Our collaborators at Michigan Medicine are in the process of collecting circulating immune cells from COVID-19 patients in different groups, including a very special high-risk group of patients who received lung or heart transplant and recovered from COVID-19,” said Wen.
If researchers can understand the details of how these immune responses differ, it may be possible to nudge the excessive responses toward becoming more like the effective ones. It may also be possible to intercede before the disease becomes severe.
In addition to helping shed light on COVID-19 now, Wen is developing a vaccine using virus-like particles. Two vaccines based on virus-like particles are currently on the market, for hepatitis B and human papilloma virus (HPV).
One advantage of vaccines made with virus-like particles is that they are safer to make and receive: at no point in the manufacturing process is the live virus involved, unless you count the initial genetic sequencing. The other is that the vaccine can be designed to train the immune system to target a more constant part of a mutating virus. For example, proponents of virus-like particle vaccines believe it is possible to design a flu vaccine that needs to be taken only once every five years, and which covers all the strains in circulation most of the time.
“One challenge is the speed and scalability of the system for making virus-like particles,” said Wen. “Especially in a pandemic, you can’t just make a tiny amount of vaccine. You have to be able to produce it on a large scale, very rapidly. That requires the engineering of a particular cellular system.”
Source: Read Full Article