Type 1 diabetes mellitus (T1DM) results from an irreversible autoimmune destruction of insulin-producing pancreatic β-cells requiring life-long substitution of insulin. In a new study, researchers at the Institute of Industrial Science, The University of Tokyo discovered that the diameter of cell-laden hydrogels determines its longevity after transplantation, paving the way for efficacious cell therapy for T1DM.
Current treatment strategies for T1DM focus on timed exogenous insulin administration, posing a significant burden on the patient as well as the health care system. Cell therapy aims at replacing lost pancreatic β-cells permanently, eliminating the need for insulin substitution. Although cell replacement therapy has been regarded as an attractive option for T1DM, its clinical success has been limited by immune-mediated foreign body reactions.
“Cell therapy suffers from a similar fate to that of organ transplantation, which is transplant rejection,” says corresponding author of the study Shoji Takeuchi. “One way to mitigate this issue is to encapsulate pancreatic cells in hydrogels, although this does not prevent the transplant from foreign body reactions. We wanted to investigate how we can optimize hydrogels to provide long-term immunoprotection for transplanted cells.”
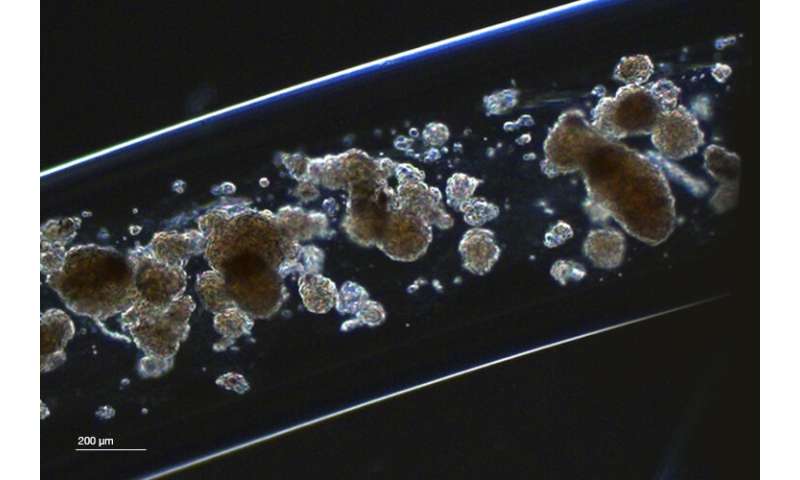
The researchers hypothesized that the diameter of hydrogel fibers critically determines whether the cell transplant mitigates foreign body reactions. By implanting barium alginate (Ba-Alg) hydrogels with variable fiber diameters into normal mice, they showed that the threshold, above which immune reactions were significantly lower, appears to be at 1.0 mm. To investigate if the biological superiority comes at a biophysical expense, the researchers compared 1.0-mm- and 0.35-mm-thick Ba-Alg hydrogel fibers. Not only was the 1.0-mm-thick fiber easier to handle than the 0.35-mm-thick construct based on biomechanical measurements, it also allowed small molecules like glucose, insulin and oxygen to pass through the hydrogel membrane, all of which are required if cells encapsulated within the hydrogel are to function properly.
But did it keep its promise to facilitate cell therapy for T1DM? To address this, the researchers loaded rat pancreatic islet cells into 1.0-mm- and 0.35-mm-thick hydrogel fibers and tested how well the fibers performed in secreting insulin upon stimulation with glucose. Although cells in 0.35-mm-thick hydrogels performed better, cells in 1.0-mm-diameter-fibers functioned sufficiently well to test them in diabetic mice in the next step. Here, the researchers transplanted the two types of hydrogels in the intraperitoneal cavities of diabetic mice and measured daily non-fasting blood glucose levels. Strikingly, 1.0-mm-thick fibers normalized blood glucose levels of diabetic mice for a period over four times longer than 0.35-mm-thick fibers, suggesting a higher longevity of pancreatic cells encapsulated in thicker hydrogel fibers. Further, microscopic analysis showed no evidence of foreign body reactions of 1.0-mm-thick fibers, while 0.35-mm-thick fibers seemed to have deteriorated over time.
Source: Read Full Article