
Desperate to solve the deadly conundrum of COVID-19, the world is clamoring for fast answers and solutions from a research system not built for haste.
The ironic, and perhaps tragic, result: Scientific shortcuts have slowed understanding of the disease and delayed the ability to find out which drugs help, hurt or have no effect at all.
As deaths from the coronavirus relentlessly mounted into the hundreds of thousands, tens of thousands of doctors and patients rushed to use drugs before they could be proved safe or effective. A slew of low-quality studies clouded the picture even more.
“People had an epidemic in front of them and were not prepared to wait,” said Dr. Derek Angus, critical care chief at the University of Pittsburgh Medical Center. “We made traditional clinical research look so slow and cumbersome.”
It wasn’t until mid-June—nearly six months in—when the first evidence came that a drug could improve survival. Researchers in the United Kingdom managed to enroll one of every six hospitalized COVID-19 patients into a large study that found a cheap steroid called dexamethasone helps and that a widely used malaria drug does not. The study changed practice overnight, even though results had not been published or reviewed by other scientists.
In the United States, one smaller but rigorous study found a different drug can shorten recovery time for seriously ill patients, but many questions remain about its best use.
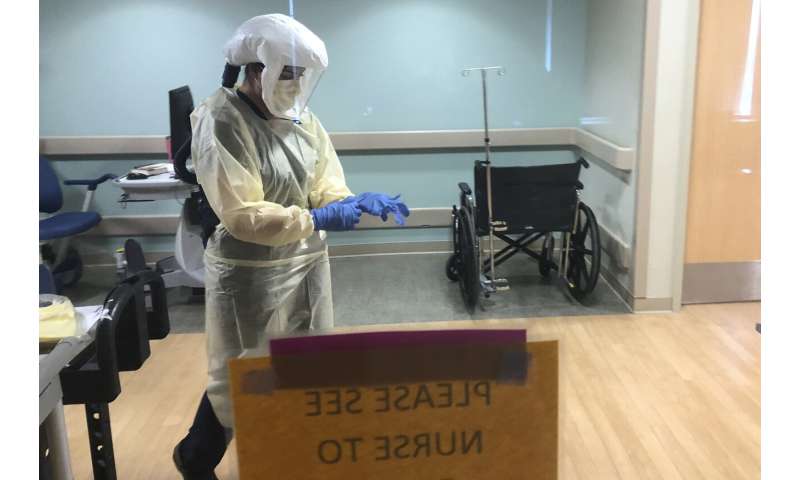
Doctors are still frantically reaching for anything else that might fight the many ways the virus can do harm, experimenting with medicines for stroke, heartburn, blood clots, gout, depression, inflammation, AIDS, hepatitis, cancer, arthritis and even stem cells and radiation.
“Everyone has been kind of grasping for anything that might work. And that’s not how you develop sound medical practice,” said Dr. Steven Nissen, a Cleveland Clinic researcher and frequent adviser to the U.S. Food and Drug Administration. “Desperation is not a strategy. Good clinical trials represent a solid strategy.”
Few definitive studies have been done in the U.S., with some undermined by people getting drugs on their own or lax methods from drug companies sponsoring the work.
And politics magnified the problem. Tens of thousands of people tried a malaria medicine after President Donald Trump relentlessly promoted it, saying, “What have you got to lose?” Meanwhile, the nation’s top infectious disease expert, Dr. Anthony Fauci, warned “I like to prove things first.” For three months, weak studies polarized views of hydroxychloroquine until several more reliable ones found it ineffective.

“The problem with ‘gunslinger medicine,’ or medicine that is practiced where there is a hunch … is that it’s caused society as a whole to be late in learning things,” said Johns Hopkins University’s Dr. Otis Brawley. “We don’t have good evidence because we don’t appreciate and respect science.”
He noted that if studies had been conducted correctly in January and February, scientists would have known by March if many of these drugs worked.
Even researchers who value science are taking shortcuts and bending rules to try to get answers more rapidly. And journals are rushing to publish results, sometimes paying a price for their haste with retractions.
Research is still chaotic—more than 2,000 studies are testing COVID-19 treatments from azithromycin to zinc. The volume might not be surprising in the face of a pandemic and a novel virus, but some experts say it is troubling that many studies are duplicative and lack the scientific rigor to result in clear answers.
“Everything about this feels very strange,” said Angus, who is leading an innovative study using artificial intelligence to help pick treatments. “It’s all being done on COVID time. It’s like this new weird clock we’re running on.”
Here is a look at some of the major examples of “desperation science” underway.
A MALARIA DRUG GOES VIRAL
To scientists, it was a recipe for disaster: In a medical crisis with no known treatment and a panicked population, an influential public figure pushes a drug with potentially serious side effects, citing testimonials and a quickly discredited report of its use in 20 patients.
Trump touted hydroxychloroquine in dozens of appearances starting in mid-March. The Food and Drug Administration allowed its emergency use even though studies had not shown it safe or effective for coronavirus patients, and the government acquired tens of millions of doses.
Trump first urged taking it with azithromycin, an antibiotic that, like hydroxychloroquine, can cause heart rhythm problems. After criticism, he doubled down on giving medical advice, urging “You should add zinc now … I want to throw that out there.” In May, he said he was taking the drugs himself to prevent infection after an aide tested positive.

Many people followed his advice.
Dr. Rais Vohra, medical director of a California poison control center, told of a 52-year-old COVID-19 patient who developed an irregular heartbeat after three days on hydroxychloroquine – from the drug, not the virus.
“It seems like the cure was more dangerous than the effects of the disease,” Vohra said.
Studies suggested the drug wasn’t helping, but they were weak. And the most influential one, published in the journal Lancet, was retracted after major concerns arose about the data.
Craving better information, a University of Minnesota doctor who had been turned down for federal funding spent $5,000 of his own money to buy hydroxychloroquine for a rigorous test using placebo pills as a comparison. In early June, Dr. David Boulware’s results showed hydroxychloroquine did not prevent COVID-19 in people closely exposed to someone with it.
A UK study found the drug ineffective for treatment, as did other studies by the U.S. National Institutes of Health and the World Health Organization.
Boulware’s colleague, Dr. Rahda Rajasingham, aimed to enroll 3,000 health workers in a study to see if hydroxychloroquine could prevent infection, but recently decided to stop at 1,500.
When the study started, “there was this belief that hydroxychloroquine was this wonder drug,” Rajasingham said. More than 1,200 people signed up in just two weeks, but that slowed to a trickle after some negative reports.
“The national conversation about this drug has changed from everyone wants this drug … to nobody wants anything to do with it,” she said. “It sort of has become political where people who support the president are pro-hydroxychloroquine.”
Researchers just want to know if it works.
LEARN AS YOU GO
In Pittsburgh, Angus is aiming for something between Trump’s “just try it” and Fauci’s “do the ideal study” approach.
In a pandemic, “there has to be a middle road, another way,” Angus said. “We do not have the luxury of time. We must try to learn while doing.”
The University of Pittsburgh Medical Center’s 40 hospitals in Pennsylvania, New York, Maryland and Ohio joined a study underway in the United Kingdom, Australia and New Zealand that randomly assigns patients to one of dozens of possible treatments and uses artificial intelligence to adapt treatments, based on the results. If a drug looks like a winner, the computer assigns more people to get it. Losers are quickly abandoned.
The system “learns on the fly, so our physicians are always betting on the winning horse,” Angus said.
A small number of patients given usual care serve as a comparison group for all of the treatments being tested, so more participants wind up getting a shot at trying something.
Mark Shannon, a 61-year-old retired bank teller from Pittsburgh, was the first to join.
“I knew that there was no known cure. I knew that they were learning as they went along in many cases. I just put my trust in them,” he said.
Shannon, who spent 11 days on a breathing machine, received the steroid hydrocortisone and recovered.
Doris Kelley, a 57-year-old preschool teacher in Ruffs Dale, southeast of Pittsburgh, joined the study in April.

“It felt like someone was sitting on my chest and I couldn’t get any air,” Kelley said of COVID-19.
She has asthma and other health problems and was glad to let the computer choose among the many possible treatments. It assigned her to get hydroxychloroquine and she went home a couple days later.
It’s too soon to know if either patient’s drug helped or if they would have recovered on their own.
THE BUMPY ROAD TO REMDESIVIR
When the new coronavirus was identified, attention swiftly turned to remdesivir, an experimental medicine administered through an IV that showed promise against other coronaviruses in the past by curbing their ability to copy their genetic material.
Doctors in China launched two studies comparing remdesivir to the usual care of severely and moderately ill hospitalized patients. The drug’s maker, Gilead Sciences, also started its own studies, but they were weak—one had no comparison group and, in the other, patients and doctors knew who was getting the drug, which compromises any judgments about whether it works.
The NIH launched the most rigorous test, comparing remdesivir to placebo IV treatments. While these studies were underway, Gilead also gave away the drug on a case-by-case basis to thousands of patients.
In April, Chinese researchers ended their studies early, saying they could no longer enroll enough patients as the outbreak ebbed there. In a podcast with a journal editor, Fauci gave another possible explanation: Many patients already believed remdesivir worked and were not willing to join a study where they might end up in a comparison group. That may have been especially true if they could get the drug directly from Gilead.
In late April, Fauci revealed preliminary results from the NIH trial showing remdesivir shortened the time to recovery by 31%—11 days on average versus 15 days for those just given usual care.
Some criticized releasing those results rather than continuing the study to see if the drug could improve survival and to learn more about when and how to use it, but independent monitors had advised that it was no longer ethical to continue with a placebo group as soon as a benefit was apparent.

Until that study, the only other big, rigorous test of a coronavirus treatment was from China. As that country rushed to build field hospitals to deal with the medical crisis, doctors randomly assigned COVID-19 patients to get either two HIV antiviral drugs or the usual care and quickly published results in the New England Journal of Medicine.
“These investigators were able to do it under unbelievable circumstances,” the journal’s top editor, Dr. Eric Rubin, said on a podcast. “It’s been disappointing that the pace of research has been quite slow since that time.”
WHY SCIENCE MATTERS
By not properly testing drugs before allowing wide use, “time and time again in medical history, people have been hurt more often than helped,” Brawley said.
For decades, lidocaine was routinely used to prevent heart rhythm problems in people suspected of having heart attacks until a study in the mid-1980s showed the drug actually caused the problem it was meant to prevent, he said.
Alta Charo, a University of Wisconsin lawyer and bioethicist, recalled the clamor in the 1990s to get insurers to cover bone marrow transplants for breast cancer until a solid study showed they “simply made people more miserable and sicker” without improving survival.
Writing in the Journal of the American Medical Association, former FDA scientists Drs. Jesse Goodman and Luciana Borio criticized the push to use hydroxychloroquine during this pandemic and cited similar pressure to use an antibody combo called ZMapp during the 2014 Ebola outbreak, which waned before that drug’s effectiveness could be determined. It took four years and another outbreak to learn that ZMapp helped less than two similar treatments.
During the 2009-2010 swine flu outbreak, the experimental drug peramivir was widely used without formal study, Drs. Benjamin Rome and Jerry Avorn of Brigham and Women’s Hospital in Boston noted in the New England Journal. The drug later gave disappointing results in a rigorous study and ultimately was approved merely for less serious cases of flu and not severely ill hospitalized patients.
Source: Read Full Article