The coronavirus SARS-CoV-2 can infect various body tissues. While the detection of the virus in the nasopharynx is established as a diagnostic method, the amount of virus found there does not allow a prognosis of the course of the disease. In a recent study, a research team from the Helmholtz Center for Infection Research (HZI) in cooperation with the University of Rijeka, Croatia, investigated the correlation between the viral load in different tissues and the mortality of patients with a severe course of COVID-19.
The researchers show for the first time that viral load can contribute to clinical prognosis, as a higher viral load in the lungs at the time of ventilation correlates with an increased risk of death. In this interview, first author Henrike Maaß and study leader Prof Luka Cicin-Sain, head of the department “Viral Immunology” at HZI, talk about the research results that were published in the journal Viruses.
You studied the viral load in different clinical samples from ventilated COVID-19 patients. What does viral load reveal about the clinical prognosis of patients? For which group of people does this apply?
Henrike Maaß: Unfortunately, a clear clinical prognosis is not possible based on the viral load alone. Especially in serum samples, the viral load can only be detected in particularly severely ill patients, as the virus first replicates in the upper and lower respiratory tract. Nevertheless, our data show that viral load can be used to identify which patients are likely to have a severe course of the disease and therefore need additional treatment.
Luka Cicin-Sain: We have seen this correlation in patients with severe disease, where lung sampling has not been an additional burden for the patient. Due to ethical considerations and patient care, we could not obtain such samples from the lungs in people with a milder course of the disease and then also not evaluate them. In these patients, the viral load can still be measured in the blood serum. As a rule of thumb, the patients with a very severe course showed a detectable viral titer in the bloodstream.
What kind of samples did you examine in the study? Are there any special aspects to be taken into account?
HM: In the study, on the one hand, we examined serum samples and, on the other hand, samples from the broncho-alveolar lavage (BAL). The special thing about BAL samples is that they come directly from the lungs. The lungs are rinsed with saline solution and the fluid is then aspirated. Since this procedure is much more complicated and elaborate than that for serum samples, this type of sample is not used very often. Fortunately for us, in Croatia these samples are used as a diagnostic tool to identify infections with bacterial lung pathogens, which allowed us to use these samples for our study. Another point is that since BAL fluids come directly from the lungs—the compartment where the virus replicates—they are highly infectious, unlike blood. To analyze this material, we worked in the S3 laboratory at HZI. This laboratory meets the high safety standards for working with such infectious samples.
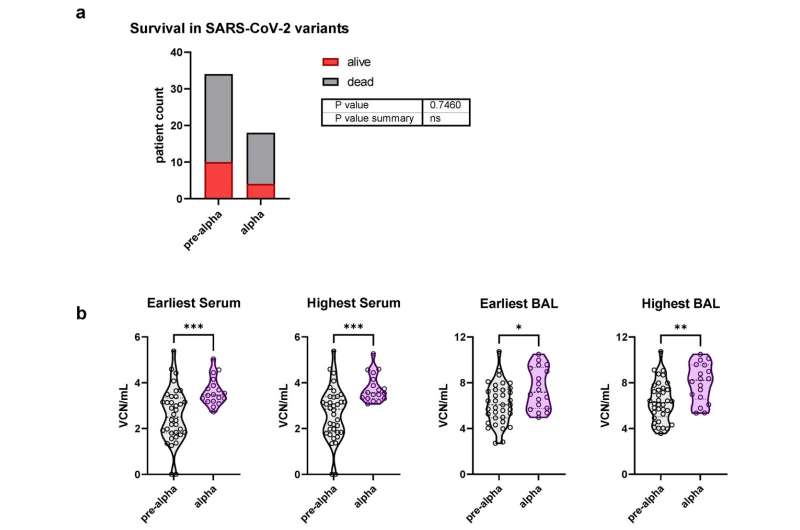
The clinical samples were taken in the second and third corona waves in Croatia. Which virus variants were predominant at the time and were there differences between the variants?
HM: At the time of the second wave, there were mainly SARS-CoV-2 variants now called pre-alpha. At the time of the third wave, the virus variant alpha was dominant. In most of our analyses, we combined the two cohorts. However, in a separate analysis, we found that alpha-infected patients had a higher viral load, both in serum and in BAL samples. In the near future, we will do further studies with delta-infected patient samples and then see how this variant compares to the previous ones. Preliminary results from these patients also show that the viral load in patients who died from the infection is higher than that of survivors.
How could these study results improve the treatment of COVID-19?
Source: Read Full Article