In the early months of the COVID-19 pandemic, markedly different scenarios played out in countries around the world. In northern Italy, the viral disease spread quickly and overwhelmed one of the world’s most developed health systems. In South Korea, where intensive contact tracing and isolation protocols were rapidly put in place after an initial surge, numbers of new cases dropped.
The difference in these outcomes cannot be explained by the absence of a specific therapeutic or diagnostic tool in Italy, or by a difference in host or pathogen biology in South Korea, said Paul Farmer, head of the Department of Global Health and Social Medicine in the Blavatnik Institute at Harvard Medical School and Kolokotrones University Professor.
The difference in outcomes, he said, is due to the social, political, cultural and historical factors that shaped responses to the contagion.
“We are not able to explain such dramatic variation from province to province or nation state to nation state by using any kind of essentialism about the host or the pathogen,” Farmer said in a recent HMS forum. “Case fatality rates have not declined or remained low because of specific preventives or therapies. It really has to do with the social responses to the disease.”
The most important thing to note about the variability in case fatality rates, Farmer noted, is that even in the absence of a specific vaccine or therapeutic to combat the novel coronavirus infection, there are effective social strategies that can be employed to protect health and slow down the spread of disease.
“There’s a lot of room for improvement,” Farmer said. “There’s a lot we can do to save lives.”
Farmer made the observations at a panel discussion of faculty members from the Department of Global Health and Social Medicine who gathered by teleconference March 26 to discuss the value of a social medicine perspective for responding to outbreaks. This panel was part of an ongoing seminar series on COVID-19 response hosted by the department. The sessions are being recorded and will be made available online.
What can be done to save lives while the world waits for the development of specific therapies, and researchers and clinicians race to learn more about this new threat to human health?
Drawing on decades of experience working with outbreaks of disease under challenging circumstances in places like Haiti, Uganda, Peru and Siberia, the HMS faculty shared insights into what works when trying to develop effective strategies to respond to both communicable and noncommunicable diseases.
They said what’s needed most is a variety of interwoven strategies, such as integrated health systems that combine prevention and treatment, from the communities where people live to the most sophisticated hospitals available. They called for improved systems to deliver the latest diagnostic and therapeutic tools where they are needed most, and a recognition that social forces have a direct impact on the viability of any preventive or clinical measure. They also cited a collaborative way of working that strengthens local resources for research, education and care delivery.
Social factors shape the curve
Megan Murray, the Ronda Stryker and William Johnston Professor of Global Health and director of the Global Health and Social Medicine research core, presented a history of the COVID-19 outbreak, including an outline of what is known about disease symptoms, progression and infectiousness and current approaches to treatment. She also described the challenges of modeling the trajectory of the outbreak and highlighting both the biological factors and the social factors that play a role in determining how the outbreak unfolds.
One of the difficulties in attempting to slow the spread of the disease is that people who are infected can transmit the virus before they develop symptoms, she said, which makes it hard to isolate individuals before they spread the disease.
In the absence of the ability to test and isolate people before they become infectious, broad programs of social distancing are necessary to slow the spread of the disease, buying time to improve diagnostics, find treatments, possibly develop vaccines and space out the need for ICUs, Murray said.
“But we can’t social distance forever,” Murray said. “We have to really consider what happens when we relax social distancing measures.”
“You could relax measures for people who are immune, but only if you know who is immune,” she said, noting that as yet there are no reliable tests for immunity readily available.
Murray added that so far, most of what’s known about the COVID-19 outbreak comes from higher-income countries with well-developed health infrastructures. She said it will be difficult to predict what will happen when the virus spreads in low- and middle-income countries.
If COVID-19 behaves like most seasonal flus, and if it behaves as laboratory experiments suggest it will, the spread of the virus may slow in warmer, humid weather and in tropical regions, Murray said. The age distribution in Africa, where 50 percent of the population is under 20, may also serve to reduce the impact of the disease there.
On the other hand, she noted, the flu pandemic of 1918, which was largely a cold weather illness elsewhere, had its worst outbreaks in West Africa in the heat of August. The social and clinical conditions in most low-income countries suggest that these countries may struggle with COVID-19 even in warm weather.
“We have to think about all of the other comorbidities,” Murray added, citing very high incidences of smoking and biomass fuel exposure in lower-income countries, which may worsen COVID-19 outcomes, and the largely unknown effect that living with TB, HIV, malaria and other infections will have on COVID-19 outcomes.
Health system capacity will also be a crucial factor in determining the course of the disease in low-resourced countries.
“Most of the countries we’re thinking about in Africa and throughout the world have almost no capacity for ICU beds, ventilators, isolated spaces within ICUs, and staff to take care of patients,” Murray said. In low-resourced settings, she said, “the currently reported in-hospital ICU mortality rates of 50 percent to date will likely be closer to 100 percent because we really just don’t have the ICU beds.”
Infectious outbreaks amplify inequality
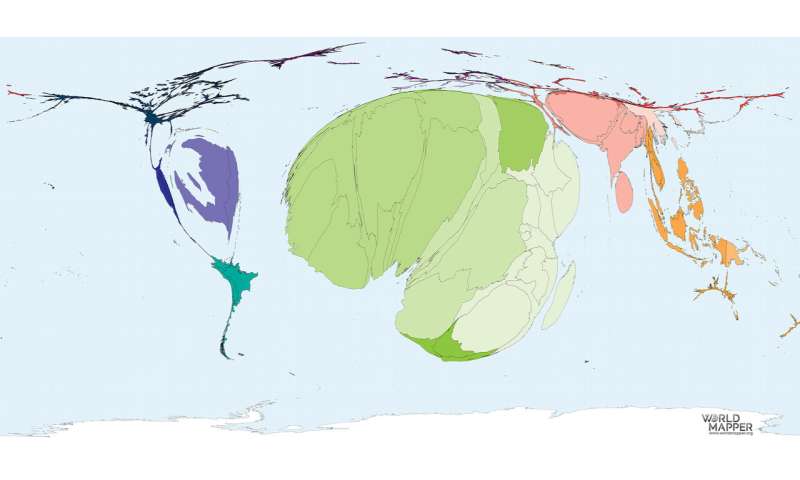
Louise Ivers, executive director of the Massachusetts General Hospital Center for Global Health and an associate professor of global health and social medicine at HMS, echoed many of Murray’s concerns as she spoke about how pandemics tend to mirror and amplify existing inequalities.
She also provided insights into where the pandemic will hit the hardest: among the poor, the already ill and those whose livelihoods are already precarious. Poverty will prevent people in these groups from complying with physical distancing protocols because if they don’t work on a given day they won’t eat. They are also unlikely to have access to clean water or soap to wash their hands, she said.
Ivers is an infectious disease physician and a special advisor for Partners In Health, where she pioneered efforts to administer a cholera vaccine in Haiti in the midst of an epidemic.
Even for diseases with known treatments, lower-income countries tend to do without, Ivers noted.
“Discovery and delivery have never just trickled down without a lot of advocacy and intervention,” Ivers said. “We’re going to have to be very proactive to make sure that those vaccines are available for all people who need them.”
One of the great ironies of global health is that often where the burden of disease is greatest, the fewest care providers are available, Ivers said.
As an example, she cited research showing that in Haiti there are .2 doctors per 1,000 people and in Uganda less than .1 per 1,000, whereas in the U.S., the average is 2.56 physicians per 1,000.
Even within the U.S., Ivers said, there are great disparities between rural and urban regions, with 3.1 doctors per 1,000 on average in urban settings, versus an average of 1.3 doctors per 1,000 in rural settings. In metropolitan Boston, there are 16 doctors for every 1,000 people
These disparities will likely drive up the toll of the coronavirus outbreak in underresourced locations, both within the U.S. and around the world, Ivers said.
While the current outbreak presents a marked challenge, Ivers emphasized that she has seen many positive things happen already that had previously been deemed impossible.
“We need to believe in what it is possible to do,” Ivers said. “And we need to look not only at the fragilities of health systems around the world, but also at their strengths. The solution to so many of our problems is in the communities where the problems are being faced.”
Ivers listed a few components that she believes will be crucial for confronting coronavirus successfully in vulnerable populations:
- Rapid scale-up of point-of-care testing and diagnostics
- Inclusion of low-income settings in emergency research
- Involvement of researchers from low-income countries
“Talent is equally distributed, but resources are not,” she said.
She also emphasized that any successful intervention must also include support to provide food and shelter for economically vulnerable populations to make social distancing possible and slow the flood of new cases.
Building a solid foundation for health, resiliency, security
While insecurity, poverty, war and political instability make outbreaks worse, improving health care systems to fight epidemics can also improve security at the individual, community, national and global levels, said Vanessa Kerry, an HMS associate professor of medicine at Mass General and the director of the HMS Program in Global Public Policy and Social Change.
The sudden, intense global focus on stemming the coronavirus pandemic is also providing opportunities to make lasting improvements to health, security and prosperity, Kerry said. By building more resilient health care systems that will be better prepared to respond to the next pandemic, more communities will be able to handle the chronic health care crises they routinely confront, such as the epidemics of premature mortality that plague mothers and infants around the world,
The best way to confront the new coronavirus is to invest in people and equipment, and to surface the local solutions that will come from people who are “living the data every day,” said Kerry. In this way, she said, countries can build foundations for resilient, integrated health care systems and “unlock and unleash that potential in a way that is enduring and holistic.”
Source: Read Full Article