Three commonly prescribed statins are best placed to lower all the “bad” types of cholesterol and prevent cardiovascular disease in people with diabetes, according to a statistical combination of the results of 42 clinical trials. The study was carried out by University of Manchester, Manchester University NHS Foundation Trust (MFT) and Keele University scientists, and funded by the National Institute for Health Research (NIHR).
It is the first study to show the effectiveness of statins, a group of medicines that can help in lowering all types of bad cholesterol for patients with diabetes, which is in line with official guidance recently updated by the National Institute for Health and Care Excellence (NICE).
Bad cholesterol in the blood, known as non-high-density lipoprotein cholesterol (non-HDL-C), can build up within the walls of blood vessels, putting people at risk of dangerous blood clots.
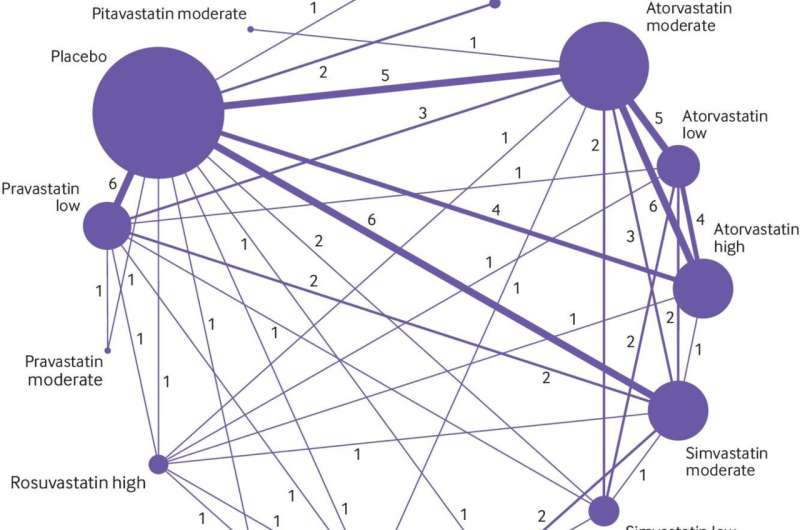
For the first time, the meta-analysis of more than 20,000 adults evaluated the effectiveness of seven statins on lowering non-HDL-C levels, and is published in the British Medical Journal.
Scientists already know which of the seven statins reduce low-density lipoprotein cholesterol (LDL-C). However, until the study, they did not know which reduced non-HDL-C, which measures LDL-C and the other types of bad cholesterol.
Therefore, non-HDL-C is a more powerful risk predictor for cardiovascular disease and has now become the primary target for reducing cardiovascular risk with cholesterol lowering treatments. Non-HDL-C can be simply calculated by doctors at no additional cost by subtracting HDL-C (or “good cholesterol”) level from the total cholesterol level.
Rosuvastatin administered at moderate and high doses, and Simvastatin and Atorvastatin administered at high doses were the most effective treatments in patients with diabetes by using non-HDL-C as a primary measure. The drugs lead to between a 2.20 to 2.31 millimoles per liter (mmol/l) reductions in non-HDL-C over 12 weeks.
In patients at high-risk of major adverse cardiac events, Atorvastatin administered at high doses was the most effective at reducing non-HDL-C by around 2.0 mmol/l.
The findings firmly support and extend new NICE guidelines for adults with diabetes, which were updated in April 2021.
NICE was the first in the UK to recommend the use non-HDL-C rather than LDL-C as a better way to measure CVD risk reduction when using cholesterol lowering treatments. However, NICE does not endorse the three drugs specifically, which is why, say the team, the analysis is important because it ranks the statins best at lowering all bad cholesterol using the preferred non-HDL-C target. It also tells us specifically that certain doses of three statins are more favorable in patients with diabetes.
Lead author Dr. Alexander Hodkinson, a health data scientist from The University of Manchester, said: “Patients with type 2 diabetes, which will affect 380 million people worldwide by 2025, are at increased risk of cardiovascular disease. Statins are considered the cornerstone of cardiovascular disease prevention by helping to lower the levels of cholesterol in the blood. They have been found to be the most effective agents in reducing the risk of coronary heart disease in patients with diabetes.
“However, we suggest that clinicians should, as NICE suggests, use all bad types of cholesterol—or the level of non-HDL-C—as a more powerful measure of cardiovascular risk. It’s simple to calculate and represents little additional workload. By using non-HDL-C as a primary measure, we found that the three statins—Rosuvastatin, Simvastatin and Atorvastatin—were ranked most effective in the meta-analysis.”
Martin Rutter is a Professor of Cardiometabolic Medicine at The University of Manchester and an Honorary Consultant Physician at the Diabetes, Endocrinology and Metabolism Centre within Manchester Royal Infirmary, part of MFT.
Source: Read Full Article