Most non-hospitalized COVID-19 “long-haulers” at the Northwestern Medicine Neuro COVID-19 Clinic continued to experience symptoms such as brain fog, numbness and tingling, headache, dizziness, blurred vision, tinnitus and fatigue an average of 15 months after disease onset, according to a new study published in Annals of Clinical and Translational Neurology.
Scientists analyzed patients six to nine months after their initial visit to the Neuro COVID-19 Clinic and discovered heart rate, blood pressure variation and gastrointestinal symptoms increased in so-called long-haulers, while loss of taste and smell decreased overall.
“This new study is novel and reports the longest follow-up period of neurologic symptoms impacting non-hospitalized patients suffering from long-COVID anywhere in the world,” said Igor Koralnik, MD, chief of Neuro-infectious Diseases and Global Neurology in the Department of Neurology, who oversees the Neuro COVID-19 Clinic. “We were surprised by the persistence of most of the debilitating neurologic symptoms of our patients, and by the late appearance of symptoms that suggest dysfunction of the autonomic nervous system.”
Scientists studied patients evaluated initially between May and November 2020 who had mild initial COVID-19 symptoms—transient cough, sore throat, etc.—and were never required to be hospitalized for pneumonia or low oxygen levels.
Of the 52 patients who completed the follow-up study, the average age was 43, 73% were female, 77% received a COVID-19 vaccine, and most continued to experience neurologic symptoms, fatigue and compromised quality of life 11–18 months after disease onset, on average 15 months.
Overall, there was no significant change in the frequency of most neurologic symptoms between first and follow-up appointments including numbness/tingling (69 vs. 65%), headache (67 vs. 54%), dizziness (50 vs. 54%), blurred vision (34 vs. 44%), tinnitus (33 vs. 42%) and fatigue (87 vs. 81%).
While loss of taste (63 vs. 27%) and smell (58 vs. 21%) decreased overall, heart rate and blood pressure variation (35 vs. 56%) and gastrointestinal symptoms (27 vs. 48%) increased at follow-up.
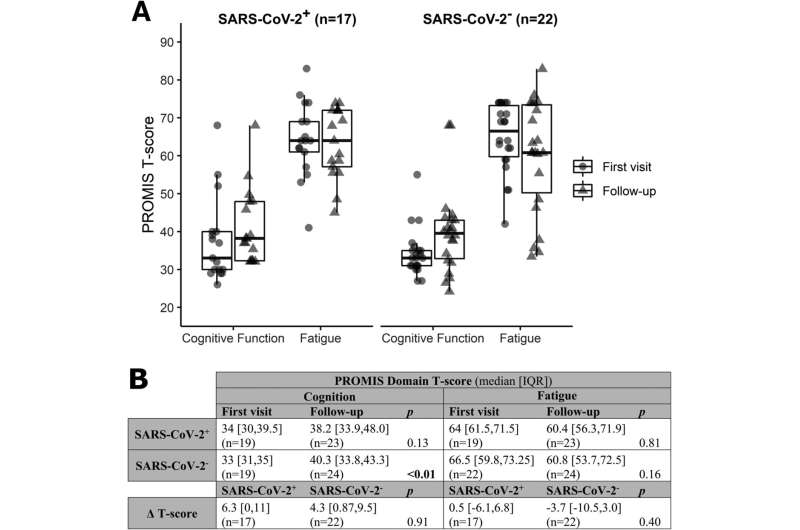
Patients reported improvements in their recovery, cognitive function, and fatigue, but quality of life measures remained lower than the average population of the United States. Seventy-seven percent of the patients were vaccinated for COVID-19, but the vaccine didn’t have a positive or detrimental impact on cognitive function or fatigue.
“Vaccination didn’t cure long COVID symptoms, but didn’t worsen them either, which is a reason given by some long-haulers for not getting vaccinated,” Koralnik said. “As new variants emerge and the number of patients impacted by long COVID rises, we’re now focusing our research on understanding the root cause of long COVID. We’re also devising interventions to improve the management of those patients and find the best treatment options for them.”
Source: Read Full Article