Surgical removal of the primary tumor is usually not enough. One in two colorectal cancer patients develops distant metastases. In about 30 percent of the cases, they appear in the lining of the abdominal cavity—the peritoneum. And that can have dire consequences. “Metastases above a certain size normally need to make space in which to grow. This in turn causes damage to organs like the liver or lungs, or behavioral abnormalities if the metastases develop in the brain. But there is plenty of room in the abdominal cavity. Here secondary tumors can proliferate undetected for a long time. And when they are discovered, they have usually already spread considerably,” says Dr. Mathias Dahlmann, a scientist at the Experimental and Clinical Research Center (ECRC), a joint institution of the Max Delbrück Center for Molecular Medicine (MDC) and Charité – Universitätsmedizin Berlin, and one of the study’s three lead authors. To ensure that patients in this advanced stage of cancer can live as long as possible, no time should be wasted on ineffective therapies. But only a close examination of the metastasis itself can determine which therapy will be the most effective.
Much research has already been done on liver and lung metastases, but little is known about peritoneal metastases. It’s time we change that, thought Professor Ulrike Stein, last author and head of the Translational Oncology of Solid Tumors Lab at the ECRC, Charité, and the MDC and Professor Beate Rau, tumor surgeon and head of the Peritoneal Carcinomatosis Center at Charité. “Patients with peritoneal metastases have the worst prognosis compared to all other metastatic sites,” Rau points out.
A single model is not enough
“As part of a project funded by the European Regional Development Fund (ERDF), we thoroughly characterized surgically removed peritoneal metastases from ten patients before bringing other research partners on board. Part of the tumor tissue was sent to EPO GmbH in Berlin-Buch immediately after removal. EPO specializes in animal models like patient-derived xenografts (PDXs). This process involves implanting small tumor cubes under the skin of mice, where they become engrafted and grow. “Mouse models, however, are relatively slow compared to cell cultures,” says Dahlmann. “It normally takes several months to obtain tumors of suitable size, and the patient sometimes dies before this can be done.” So the researchers also opted to use a second technology.
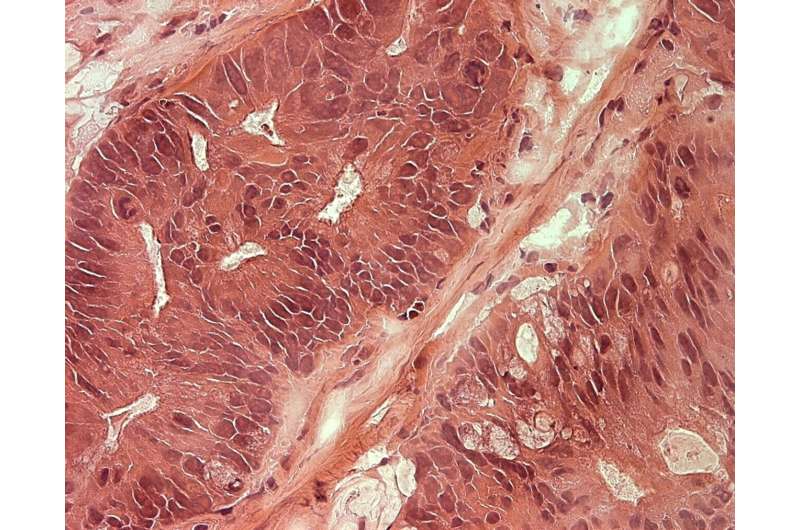
Another piece of tumor tissue was sent at the same time to CELLphenomics GmbH in order to grow organoids. The task of creating such miniature images of the tumor tissue (PDO models) requires preparing the tissue in the laboratory and embedding it in a gel-like matrix that biochemically mimics the body’s connective tissue. The tumor cells continue to grow within the matrix in such a way that the organoids mirror the architecture of the original tissue and—unlike in 2D cell cultures—can also recapitulate the heterogeneity of the tumor. This method allows any number of microscopically small versions of a patient’s tumor to be grown in a short time, and the researchers tested 17 standard therapeutics on tumors thus created.
The two model systems together provided a meaningful picture. Yet testing therapeutic agents on model systems was only one of the goals. The researchers were primarily interested in finding specific molecular markers in the cancer cells. In other words, genes that are mutated or particularly active in certain metastases that respond to treatment X, Y or Z—in order to be able to use these biomarkers to make individual therapeutic predictions.
How could the metastases be treated?
Dahlmann prepared the tissue samples from both model systems and other samples from the tumor database for the genome analyses. These were performed centrally by the German Cancer Consortium (DKTK) in Heidelberg. Proteomics specialist Dr. Philipp Mertins then set to work at the MDC to analyze the next layer: the proteins encoded by the genes. All the raw data finally ended up back with Dahlmann, who now looked for patterns and correlations in a puzzle consisting of millions of pieces.
The search paid off: he found biomarkers that could be used to predict therapy response. Severe mutations of the BRCA2 gene, which plays a key role in repairing cell damage, were discovered in 85 percent of the metastasis samples. Drug testing then showed that otherwise therapy-resistant metastases with this signature responded to a combination of the standard drug 5-FU with an additional PARP inhibitor. In others, the combination of MEK and PARP inhibitors successfully inhibited tumor growth.
A long road to the clinic
“We must not forget what cancer patients die of. In the vast majority of cases it’s not the primary tumor—but the metastases 90 percent of the time,” Stein stresses. Peritoneal metastases occur not only in colorectal cancer, but also in other solid tumors. And mutations of the BRCA2 gene are mainly known from other types of cancer—breast, ovary, stomach and prostate. Here, too, the treatment of metastases often fails.
The researchers next want to extend their studies to a larger number of tissue samples from colorectal cancer patients. If the results are confirmed, clinical trials will follow. “There is still a long way to go before patients can benefit from these discoveries. That is because the techniques to detect the molecular changes need to become much faster and even more accurate,” says Rau. “But we are on the right track.”
Source: Read Full Article