Despite the remarkable successes of immune-based treatments for cancer, not everyone responds to these approaches and relapses do occur. Researchers around the world are racing to find ways to improve outcomes for people receiving immunotherapy. But new findings from scientists at Memorial Sloan Kettering suggest they may be focusing too narrowly on the problem.
According to Ming Li, an immunologist in the Sloan Kettering Institute, most existing immunotherapy approaches, including both checkpoint blockade and CAR T therapy, aim to prod the immune system into finding and killing cancer cells—a kind of frontal attack on the disease.
But tumors also need supportive environments—safe harbors—in which to grow and thrive. “They need the support of blood vessels that provide them with nutrients,” Dr. Li says.
Could destroying these safe harbors be an indirect way to fight this internal enemy? Dr. Li thinks the answer is yes, and on October 21 he published two papers in the journal Nature in support of the concept.
“We know that the immune system is incredibly adept at recognizing harmful invaders and attacking them with precision,” he says. “But that’s not the only way our immune system protects us from threats. It also promotes healing of damaged tissue so that pathogens can’t take root in the body. This latter role, we now show, can also be enlisted in the fight against cancer.”
Dr. Li and his colleagues found they could thwart cancers in mice by encouraging immune cells to begin the process of wound repair around a tumor. In the process, blood vessels that feed the cancer are pruned away and cancer cells starve and die. It’s an approach that Dr. Li has dubbed “cancer environment immunotherapy.”
Wounds and cancer
To understand how wound healing can help curb cancer, consider what happens when someone gets an injury, say a cut from a knife. Early on, the site becomes inflamed—red, hot, and swollen. During this phase of wound healing, blood vessels dilate and immune cells rush in to fight enemies that may cause infection and clean up the debris. But later on, the wound fills in with new tissue, and inflammation resolves.
An important player in the wound healing process is a molecule called TGF-beta, whose presence waxes and wanes with the inflammation cycle. In the context of a cancerous “wound,” TGF-beta persists and makes cancer growth worse. By contrast, blocking its action inhibits tumor development. This latter effect is dependent upon immune cells called T cells, previous research has shown.
Dr. Li and his team wanted to find out more about which T cells were involved in curbing cancer growth when TGF-beta is blocked. They initially suspected that a subset of T cells called CD8 T cells, or “killer” T cells, were responsible for restraining tumor development. But when they genetically removed the receptor for TGF-beta from CD8 cells in mice, it had no effect on cancer growth.
Next, they asked whether a different subset of T cells, called CD4 T cells, or “helper” T cells, could explain the phenomenon of cancer suppression. Indeed, genetically removing the receptor for TGF-beta in CD4 T cells dramatically reduced cancer growth in mice.
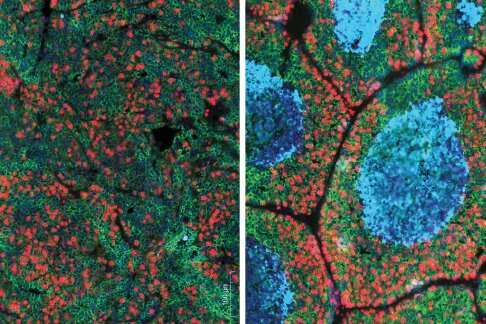
How do CD4 T cells contribute to cancer control in this context? Dr. Li and his colleagues found that these cells promote wound healing around a tumor. As part of this process, the blood vessels supplying nutrients to a tumor are dramatically remodeled, and a kind of protective wall is formed around the tumor, depriving it of sustenance.
These results, reported in the first Nature paper, showed that blocking TGF-beta signaling in CD4 T cells could activate a powerful wound healing response that directly opposes cancer development.
But what about tumors that have already been growing? Could blocking TGF-beta restrain them? Dr. Li and his team explored this question in a second set of experiments, published in a second Nature article.
They designed an antibody-based drug that can bind to both TGF-beta and T helper cells. They found that this drug, which they called 4T-Trap, could dramatically reduce cancer in mice.
Previous attempts at blocking TGF-beta as a cancer treatment have not been successful, likely because this molecule has many effects in the body and therefore blocking it completely can cause severe side effects such as heart problems or even the appearance of new cancers. But 4T-Trap targets the TGF-beta-blocking-molecule directly to CD4 T cells, so side effects are reduced. In other words, it’s a more targeted approach.
“An exciting homecoming”
That fact that CD4 T helper cells were the key players rather than CD8 killer T cells came as something of a surprise to the researchers. “These days, CD8 cytotoxic T cells that recognize cancer cells are in the spotlight.” Dr. Li says, “It’s almost become dogma that if it’s T cell mediated, then it must be CD8 T cells. That was our original hypothesis, too. But that turns out not to be the case.”
Yet the findings are not completely unprecedented. In fact, the discovery that the promotion of wound healing can dramatically curb cancer progression meshes nicely with older work. In the mid-1980s, cancer researcher Harold Dvorak published a now-famous article in the New England Journal of Medicine, in which he argued that tumors are essentially “wounds that do not heal.” Tumors enlist normal wound healing to help themselves grow. They thrive by enlisting the early stages of the immune responses to tissue damage—growth of new blood vessels, for example—but then never get to later stages of wound healing when these blood vessels are normally pruned away.
“By blocking TGF-beta in T helper cells, we allow the wound healing to run to completion,” Dr. Li says. “We heal the wound that is cancer.”
Reflecting on the way his results echo these earlier findings, Dr. Li says, “it’s an exciting homecoming.”
Source: Read Full Article