Neuroscientists at the University of Portsmouth, with collaborators in the UK and the U.S., have made a breakthrough in the study of Alzheimer’s which could inspire better treatments and earlier diagnosis.
The researchers have for the first time found a key protein in one of the brain regions first to be affected by Alzheimer’s.
The study, led by Jerome Swinny, professor of neuropharmacology at the University of Portsmouth and funded by Alzheimer’s Society, set out to fully understand how this brain region changes in the earliest phases of the disease and why.
The researchers hope the results might help to facilitate earlier diagnosis or the identification of treatments that may alter the progressive nature of the condition.
The study is published in Neuropathology and Applied Neurobiology.
Professor Swinny said: “This breakthrough provides direction for future studies focusing on developing different drugs for use at the appropriate stages of the condition.
“Until now we have used drugs that address only the symptoms of Alzheimer’s, and their effects wear off after a number of years. The use of drugs specifically designed to target the underlying early stage pathology, could help stem further progression of the disease throughout the rest of the brain, thereby enhancing the quality of life for those living with the Alzheimer’s as well as those that care for them.”
He and his colleagues focused on how the brain changes in the early stages of the condition.
This has been scientifically challenging because unequivocal diagnosis of Alzheimer’s invariably occurs only in the late stage of the condition.
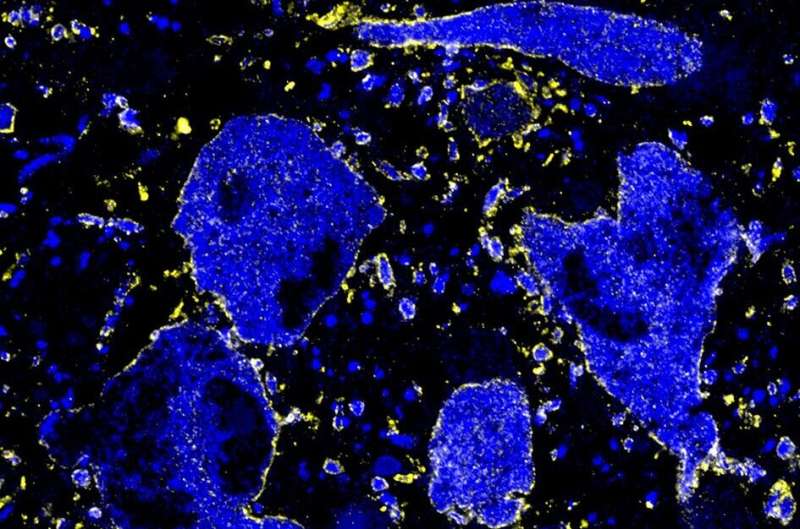
For the first time, key proteins—amyloid β oligomers (AβO) involved in Alzheimer’s pathology, were found in one of the earliest brain regions to be affected by the condition—the locus coeruleus (LC). This is significant because up until now it was believed that AβO were not a significant component of Alzheimer’s pathology within the LC, especially in the early stages.
Alzheimer’s-related pathology is first detectable in a few brain regions, long before patients exhibit any clinical symptoms. However, because it is a progressive disease, it eventually spreads throughout the brain to cause a significant degree of nerve cell loss, giving rise to the main symptoms such as changes in the way we think, remember or deal with daily emotional challenges.
What does this mean for early diagnosis?
The LC controls a number of the key brain functions that are severely compromised in Alzheimer’s, such as memory, cognition and our stress response. A large body of evidence, using brain imaging, also indicates that there are changes in the structure of the LC during Alzheimer’s. However, precisely how Alzheimer’s alters LC function, at the level of individual nerve cells, has been relatively less well understood.
This study, using an animal model of Alzheimer, provided the first demonstration that AβO, found in Alzheimer’s patients, result in the over activity of LC nerve cells. This is notable because such heightened levels of LC activity are thought to drive changes in human behavior which closely mirror those seen in the early stages of people living with Alzheimer’s, such as emotional instability and a heightened response to stress.
These findings may therefore help to explain why such behavior occurs during this phase of the condition.
Professor Swinny said: “This research is important because we can combine this knowledge on changes in LC function, with existing knowledge of its change in structure, to drive the development of improved diagnostic protocols, such as functional brain imaging, during the earliest stages of the condition. Such early, reliable diagnostic tools are essential for any patient interventions, be they new drug treatments or the optimisation of care.
What does this mean in terms of early treatment?
The scientists identified the mechanism through which AβO proteins alter LC nerve cell activity. They discovered that AβO proteins impair the function of another protein that is central to regulating how active nerve cells are in the brain. This protein is called the GABA-A alpha 3 receptor.
Dr. Louise Kelly was the lead researcher, and undertook this project as her Ph.D. in the lab of Professor Swinny. She is now an Alzheimer’s researcher at the University of Southampton.
She said: “GABA-A alpha 3 receptors are part of a class of brain chemicals that are responsible for controlling how active nerve cells become; consider them the ‘brakes of the brain.” If their function is impaired, nerve cells become too active. Apart from changing brain function, a serious consequence of such over-activity is nerve cell death, which is what we see in Alzheimer’s.
“This suggests a common mechanism for this early phase of the condition, which if targeted, perhaps through drugs which enhance their function, could help stem further progression throughout the brain, thereby enhancing the quality of life for those living with the condition.”
Finally, the team uncovered another protein that also controls the activity of LC nerve cells, but is resilient to AβO-mediated pathology. This raised the prospect of targeting them pharmacologically in order to reverse the ABO-induced changes in the LC.
Louise, says, “This protein is called the glycine transporter 1 (GlyT1). We were able to demonstrate that dugs that modulate GlyT1, are capable of reversing the over-activity of LC nerve cells due to AβO. This is important because such GlyT1 modulators are currently undergoing clinical trials, by other investigators, as cognitive enhancers in a range of other conditions, such as schizophrenia. They have been proven to be safe and therefore raise the possibility of being repurposed for other conditions which impair cognition, such as Alzheimer’s.
“It’s exciting to think we have uncovered at least two potential pathways (GABA-A alpha 3 and GlyT1) to target in terms of improving the changes that occur in the earliest stages of Alzheimer’s.
“The next phase of this research will focus on assessing which of these strategies are more effective for future treatment strategy.”
Dr. Richard Oakley, head of research at Alzheimer’s Society, said, “There’s still a lot to piece together about what’s happening in the brain in the very early stages of dementia, and what early outward signs they might cause.
“Issues with mood and emotional instability could be some of these signs—in this study funded by Alzheimer’s Society the authors suggest a really interesting hypothesis of how a key protein of Alzheimer’s—amyloid beta—may be linked to overactivity in a specific area of the brain that influences our stress response.
“Armed with more knowledge like this of these very early brain changes and their potential effect on people’s behavior, our funded researchers will be able to fast-forward the hunt for drugs to stop these brain changes in their tracks, and one day stop dementia altogether.
Source: Read Full Article