A new study by researchers at University of Illinois Chicago suggests that when the protein optineurin, or OPTN, is present in cells it restricts the spread of HSV-1, the herpes simplex virus type 1.
In a “first of its kind” study, researchers also found a potential direct connection between neurodegenerative diseases, such as Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), glaucoma, and the herpesvirus, said Dr. Deepak Shukla, the Marion H. Schenk Esq. Professor in Ophthalmology for Research of the Aging Eye, and vice chair for research at UIC.
The research paper, “OPTN is a host intrinsic restriction factor against neuroinvasive HSV-1 infection,” led by Shukla, was published recently in the journal Nature Communications.
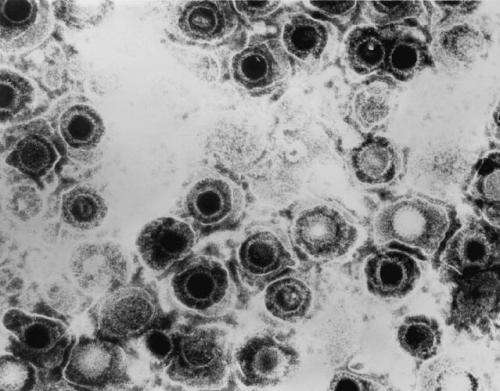
Researchers sought to discover why HSV-1 can become fatal for individuals who are immunocompromised but not for healthy individuals. Herpesviruses naturally infect the central nervous system and can result in degenerative brain and eye disorders, as well as encephalitis. However, in most individuals, the virus is suppressed during a primary infection before it can significantly damage the central nervous system.
The new research suggests why HSV-1 is suppressed: OPTN, a conserved autophagy receptor, selectively targets HSV-1 proteins to degradation by autophagy, explained Tejabhiram Yadavalli, a co-author of the study and visiting scholar at UIC’s department of ophthalmology and visual science.
“OPTN stops the virus from growing and it stops it by autophagy—engulfing the virus particles inside tiny vesicles called autophagosomes. The autophagy that happens is very selective. That has meaning for other viruses as well,” Shukla said.
The researchers believe the results from this study will apply to all eight different human herpesviruses.
For the study, mice with removed OPTN genes were infected with ocular HSV-1. The virus growth was much higher in the brains of animals without OPTN, killing local neurons and eventually leading to animal death. This shows there is a faster degeneration of neurons when OPTN is not there. Additional studies are being planned to examine naturally occurring mutations in OPTN, such as the ones reported in glaucoma and ALS patients, and how they may affect neuronal health and HSV-1 infection, Shukla explained.
“Where you have mutated OPTN plus herpes, you have the recipe to create a disaster in terms of neurodegeneration,” Shukla said.
“The study also shows there is an impairment of immune response when there is a deficiency in OPTN. OPTN is needed to signal an influx of proper immune cells at the site of infection. When you don’t have it, you have issues,” said Chandrashekhar Patil, also a co-author of the study and a visiting scholar at UIC’s department of ophthalmology and visual science.
Some of those issues could include neurodegenerative disorders, which researchers believe further research may show.
“We think we will have data to show other viruses, such as Epstein-Barr, Kaposi’s sarcoma, varicella-zoster, are all going to share this mechanism because they share homologous proteins,” Shukla said.
Because the herpesvirus sits in neurons forever, there is speculation it is connected to neurodegenerative diseases. The immune system requires inflammation to constantly fight off the virus, and neurons have some degree of damage because of this continuous immune response, according to Dr. Tibor Valyi-Nagy, professor of pathology, director of neuropathology at UIC and research collaborator on the study.
The study also showed that animals without OPTN and infected with HSV-1 after 30 days lost the ability to recognize objects. Shukla said this could be an indication that having HSV-1 along with a mutation of OPTN could accelerate neuronal damage, which would translate into cognitive impairment.
“Part of our translational research can be how can we correct the problems with OPTN so that we don’t have issues with neurodegeneration,” Shukla said.
Additional authors are Joshua Ames, Rahul Suryawanshi, James Hopkins, Alexander Agelidis, Chandrashekhar Patil and Brian Fredericks, all of UIC, and Henry Tseng of Duke University Medical Center.
Source: Read Full Article