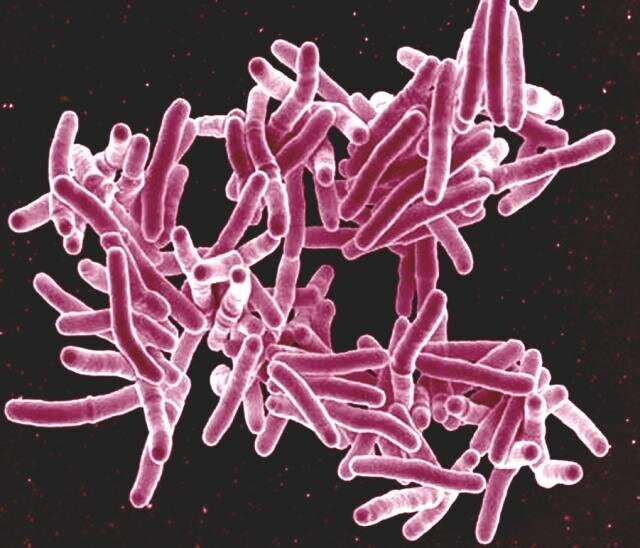
Two strains of the bacterium causing tuberculosis have only minor genetic differences, but attack the lungs in completely different fashion, according to Rutgers researchers.
The findings, published in the journal Nature Communications, could help break the cycle of rapid transmission of TB, the second-leading infectious killer in the world after COVID-19, according to the World Health Organization. The disease mechanisms uncovered in the study could also provide answers about why treatments work in some patients but not others.
“These findings implicate strain differences as having an important effect on the response of lung alveolar macrophages and how tuberculosis manifests itself in the body and how it is transmitted,” said study author Padmini Salgame, associate director of the Public Health Research Institute at Rutgers New Jersey Medical School. “We also believe it will inform anyone hoping to devise more effective treatments.”
To better understand transmission and how it relates to treatment outcomes, the researchers focused on the impact these two strains of Mycobacterium tuberculosis have on the lungs. Though the strains differ slightly in their gene sequences, one is regarded as “high transmission” because it spreads easily and the second as “low transmission” because it does not infect as readily. TB bacteria are spread through the air when persons with TB disease in their lungs cough, speak or even sing.
Using strains identified in a Rutgers collaborative study with researchers at Núcleo de Doenças Infecciosas (NDI) in Brazil comparing “high transmission” and “low transmission” households of people with TB, the scientists studied the immune pathways that the pathogen triggered in the lungs of the infected mice.
In mice infected with the high transmission strain, their lungs quickly formed clumps of immune cells known as granulomas that encased the invading bacteria, stopping development of a more virulent disease. In most cases, the granulomas broke down eventually, spilling their contents. Researchers believe that if the escaped bacteria are close enough to the bronchial airway, they could be expelled into the air as infectious aerosols.
“By inducing granulomas with the potential to develop into cavitary lesions that aid bacterial escape into the airways, high transmission M. tuberculosis strains are poised for greater transmissibility,” said Salgame, who is also a professor in the Department of Medicine.
In mice infected with the low transmission strain, the invading bacteria were slow to activate the lung alveolar macrophages and ended up producing patches of inflammation within the lungs that did not allow the bacteria to escape into airways and allowed them to conglomerate and intensify the infection, Salgame said.
The discovery of the different trajectories taken by the strains gives hope to new approaches to stopping transmission and treatment.
“We have long known that some individuals with TB are more infectious than others,” Salgame said. “However, until now, the mechanisms responsible for this variability in transmission between individuals with TB have not been well understood.”
Source: Read Full Article