Duke-NUS Medical School researchers, together with collaborators in Singapore, have designed armored immune cells that can attack recurring cancer in liver transplant patients, while temporarily evading immunosuppressant drugs patients take to avoid organ rejection. The findings were published in the journal Hepatology.
Hepatocellular carcinoma is the most common type of primary liver cancer and the sixth-most common cancer worldwide. It often develops in people with chronic liver disease following hepatitis B infection.
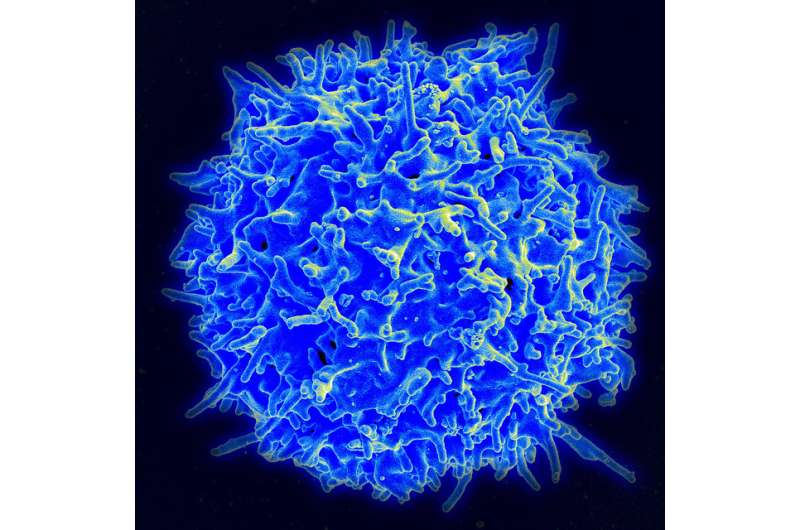
A common treatment for hepatocellular carcinoma is to completely remove the liver and replace it with a healthy one from a donor. However, hepatitis B-related hepatocellular carcinoma can recur in some patients following transplantation. To kill the cancer, doctors can inject immune cells, called T cells, which are specially designed to target hepatitis B material found in the cancer cells. However, liver transplant patients must take drugs that suppress their immune systems to prevent their bodies from attacking the transplants. This significantly hinders the effectiveness of T cell therapy.
“We developed a method to make T cells that specifically target the hepatitis B antigen in liver cancer cells while, at the same time, making them resistant to two commonly used immunosuppressants: tacrolimus and mycophenolate mofetil,” said Professor Antonio Bertoletti, senior author of the study from Duke-NUS’ Emerging Infectious Diseases Programme.
“Importantly, the resistance of our T cells to the immunosuppressants only lasted for about four days after which they regain their sensitivity to the drugs,” added Prof Bertoletti.
This transient effect, a result of the engineering approach the team used, provides an additional layer of safety to minimize the possibility of organ rejection.
Prof Bertoletti and his colleagues began their investigations by testing the effects of tacrolimus and mycophenolate mofetil on T cells designed with a special receptor that targets hepatitis B antigens located on liver cancer cells. They found that both drugs significantly reduced the T cells’ ability to kill the cancer cells.
The team then re-designed the T cells by adding genetic codes that disrupt the enzymes needed by the two drugs to suppress immune cells. They found that these ‘immunosuppressive drug resistant armored hepatitis B T cell receptor’ (IDRA HBV-TCR) T cells showed “superior killing” power of hepatocellular carcinoma cell targets for up to four days.
“We also found that this strategy can be applied to target other pathologies that commonly occur in transplant patients receiving immunosuppressive drugs, like Epstein-Barr virus and cytomegalovirus reactivations,” said Dr. Anthony T Tan, a senior research fellow in Prof Bertoletti’s lab and a co-author of the study.
“Innovative research like this lays the foundation for new discoveries and transformative change,” said Professor Patrick Casey, senior vice-dean for research, Duke-NUS Medical School. “With waiting lists for organs lengthening around the world, ensuring that those patients who benefit from a much-needed transplant can remain in remission is a significant advance and offers much hope.”
Source: Read Full Article