
Fraunhofer researchers have developed a very fast technology for determining whether a tumor has been fully removed—before the patient even leaves the operating theater. Using a combination of laser scanning microscopy and fluorescent tumor markers, doctors can detect any remaining cancer cells immediately after operations.
Surgically removing a tumor is a delicate process. The cancerous tissue must be removed in its entirety, with great precision and as few incisions as possible. Afterward, the surgeon must ask themselves a number of questions. For example, were all the cancerous cells completely removed? And did the removal damage the surrounding tissue? With brain tumors in particular, it is important to remove as few healthy nerve cells as possible.
Now, Fraunhofer researchers working in the LSC-Onco (Laser Scanning Oncology) project have found a quick, reliable solution to this problem by combining laser scanning microscopes and fluorescent tumor markers. Using the microscope, doctors can examine the tissue surrounding the area the tumor was removed from—without even leaving the operating theater. Michael Scholles, Head of the Fraunhofer Center for Micro-electronic and Optical Systems for Biomedicine MEOS, explains: “A fluorescent marker applied beforehand allows doctors to see any cancer cells that may be left behind after the incision. Then these cells can be completely removed, with great precision.” The technology was developed at the Fraunhofer Center in Erfurt, where MEOS works on key technologies in the fields of life sciences, microelectronics, optics and photonics. The project involved researchers from the Fraunhofer Institute for Photonic Microsystems IPMS in Dresden and the Fraunhofer Institute for Cell Therapy and Immunology IZI in Leipzig.
Laser scanning microscopes in the operating theater
In the LSC-Onco project, experts from Fraunhofer IPMS developed the tried and tested concept of a laser scanning microscope further, using a microscanner mirror manufactured with MEMS (micro-electro-mechanical systems) technology. Inside the microscope, the mirror oscillates at a rate of several thousand times per second, directing blue laser light with a wavelength of 488 nanometers over the entire image field point by point. The mirror simultaneously directs the fluorescent light emitted by the tissue towards a highly sensitive photodetector. The signals from the photodetector can then be used to construct a two-dimensional image. Images can also be recorded on different planes, so that tumor cells beneath the surface also become visible. “This means that, for the first time, a powerful, portable laser scanning microscope that can be positioned right next to the patient in the operating theater is a feasible reality,” says Scholles.
Fluorescent tumor markers
Before the microscope can detect cancer cells, the cells themselves must first be marked. Researchers from Fraunhofer IZI used their biomedical expertise to develop a fluorescent tumor marker liquid that, simply put, makes cancer cells glow beneath the microscope. The team from Fraunhofer IZI developed the markers for use on brain and skin tumors and are currently investigating whether other types of tumors will react similarly. The Helios Hospital Erfurt provided the tissue samples necessary for developing the tumor markers, with the consent of patients.
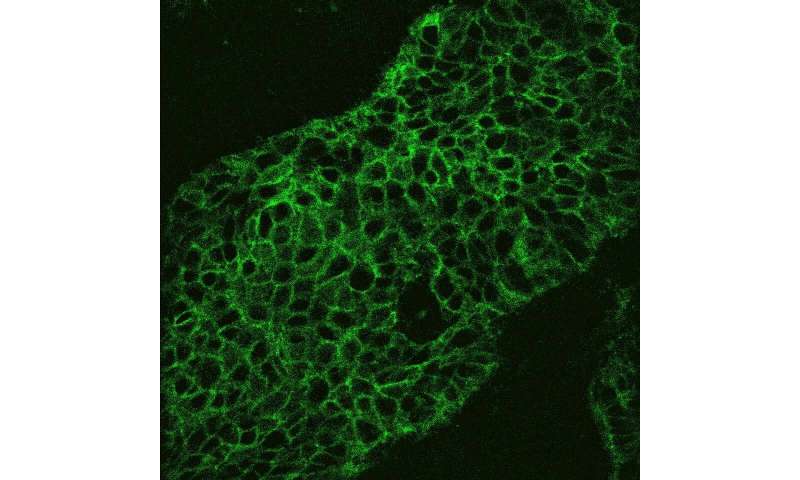
After the tumor is removed, the tumor marker is applied to the surrounding tissue and the laser scanning microscope is positioned directly above the wound. When the microscope’s blue laser beam encounters healthy cells, the reflected light is blocked by dichroic filters, which have the ability to pass only specific wavelengths. As a result, the image on the microscope display stays black for those cells. However, if the blue laser encounters cancerous cells, the tumor marker emits a fluorescent green. This light passes through the dichroic filters and appears on the display as a green dot or patch. The resolution of the system is so high that even individual cancer cells can be detected and shown on the display. “It only takes a few seconds to examine the operating field with the laser scanning microscope,” says Scholles. By referring to the image on the display, doctors can cleanly remove any remaining cancer cells (normally found at the edge of the wound) in their entirety, all without damaging the healthy tissue.
Improving patients’ chances of recovery
When compared to current practices in oncological surgery, LSC-Onco represents a huge step forward. Prior to this development, surgeons have generally taken tissue samples from the edges of the wound following the removal of a tumor and sent these samples to a hospital laboratory. After a few minutes’ wait, a diagnosis would be delivered as to whether the sample cells were cancerous. If so, the surgeon would then have to cut away more tissue. This method is very time-consuming, which adds to the strain on the patient undergoing the operation. “With LSC-Onco, all these steps can be carried out in one go during the operation, and what’s more, the precision is much greater. It also protects the surrounding tissue, because you can see exactly where the healthy tissue starts on the microscope display. And now, waiting for lab tests results is a thing of the past,” says Scholles, Head of MEOS.
Source: Read Full Article